Gallbladder pancreatitis is also known as gallstone pancreatitis, which is also called biliary pancreatitis, happens when gallstones block the bile ducts. This blockage may cause acute pancreatitis. When this happens, it causes inflammation of the pancreas and leads to abdominal pain.
This condition results in discomfort and may result in significant issues if left untreated. Identifying signs and manifestations of persistent abdominal pain is essential. Familiarizing yourself with the typical causes, symptoms, diagnostic methods, and treatment options can be very beneficial.
Key Highlights
- Gallbladder pancreatitis occurs when gallstones block the pancreatic duct. This blockage leads to swelling, or inflammation, of the pancreas.
- Symptoms such as severe stomach pain, nausea, vomiting, high body temperature (fever), and jaundice are common.
- To find out if you have this condition, doctors usually do blood tests, an ultrasound, and advanced imaging like CT scans.
- Treatment may include IV fluids, pain relief, or surgeries, such as gallbladder removal.
- Changing your eating habits, keeping at a healthy weight, and seeing your doctor regularly can all help prevent this problem.
Southlake General Surgery, led by Dr. Valeria Simone MD, focuses on personalized care for effective treatment and prevention.
Understanding Gallbladder Pancreatitis
The blockage of either the common bile duct or the pancreatic duct by gallstones causes gallbladder pancreatitis. This blockage prevents digestive enzymes from moving.
When this occurs, the pancreas becomes upset and swollen. This condition often affects people with certain risk factors, such as obesity or drinking too much alcohol.
If it is not treated, it can develop into severe acute pancreatitis and lead to serious complications. Therefore, early diagnosis and treatment are very important to manage this condition effectively.
What is Gallbladder Pancreatitis?
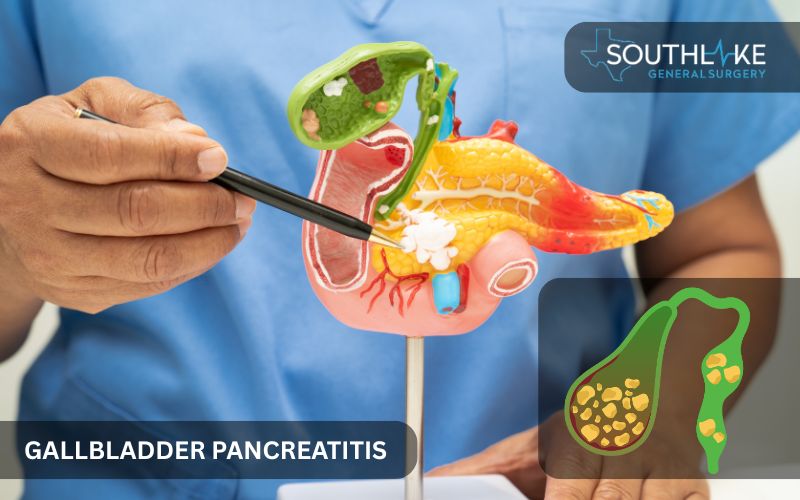
Gallbladder pancreatitis occurs when the pancreas gets inflamed because of gallstones. By obstructing passageways like the pancreatic duct or the common bile duct, these stones have the potential to cause serious health complications.
When they block these channels, it stops the flow of digestive enzymes. The accumulation of these enzymes can lead to additional complications for the pancreas. This increases your risk of experiencing severe acute pancreatitis.
The pancreas plays a key role in digestion. It produces enzymes that assist in the digestion of food within the small intestine. Furthermore, the pancreas is responsible for the production of hormones like insulin, which play an essential role in regulating blood sugar levels.
In gallbladder pancreatitis, blockages can cause these enzymes to activate too soon inside the pancreas. This early activation can increase inflammation.
In serious cases, the pancreas may not function properly, affecting pancreatic function. This can be very dangerous if you do not seek treatment. It is important to watch for early symptoms, such as sharp abdominal pain and issues with digestion.
Identifying these signs can enable you to respond promptly. Potentially, this might reduce the probability of problems stemming from gallbladder pancreatitis.
How Gallstones Cause Pancreatitis
Gallstones are solid formations that occur in the gallbladder, created from bile. They can cause pancreatitis in the gallbladder. Sometimes, these stones move through the bile ducts. When they become lodged in the common bile duct or the pancreatic duct, they have the potential to obstruct the flow.
This blockage can lead to pancreatitis in two main ways:
- Bile backwash into the pancreas: Strong bile can flow back into the pancreas. This might cause more inflammation.
- Enzymatic activation: When there is high pressure in the pancreatic duct, the digestive enzymes may start working early. This harms pancreatic tissues.
Gallstones can seriously affect the digestive system. They have the potential to cause serious inflammation and other problems. To properly understand the risks of pancreatitis, it’s essential to comprehend how gallstones obstruct the ducts.
Symptoms of Gallbladder Pancreatitis
Symptoms of gallbladder pancreatitis often begin mildly but can worsen quickly. When people first notice symptoms, they may experience nausea, vomiting, and abdominal pain. The feeling of pain might move to the back or chest region. In extreme situations, individuals may experience fever, chills, and jaundice.
These signs could indicate serious problems like pancreatic necrosis or infection. It is important to spot these symptoms early, as the symptoms of acute pancreatitis can escalate. Seeking immediate medical assistance can avert significant complications arising from acute pancreatitis.
Identifying Early Signs
Gallbladder pancreatitis often shows early signs such as:
- Nausea and vomiting that persist for an extended period can occur when gallstones lead to inflammation in the digestive system.
- Abdominal pain in the abdomen can begin as a mild discomfort. It can then change to sharp or tight pain that may move to your back, shoulder, or chest.
People need to watch for these signs after they eat fatty meals. These signs may exacerbate gallbladder problems.
Getting help with these early signs can stop the condition from getting worse. Knowing these warning signs can help you get treatment faster and prevent serious risks.
Recognizing Severe Symptoms
In serious cases, gallbladder pancreatitis can cause symptoms that need emergency treatment. These symptoms include:
- There is significant swelling in the stomach due to inflammation.
- A fever.
- Jaundice from a gallstone that is blocking the bile duct.
As the problem gets worse, you may notice signs like this:
- Fast heart rate
- Dehydration
- Severe pain
Constant vomiting can make everything more difficult. It prevents the patient from keeping food and drinks down. This makes it necessary to get quick help.
If you feel a really strong pain or feel weak, do not wait. Go get medical help immediately. This can help lower the risk of complications, like pancreatic necrosis or severe infections.
Diagnosis of Gallbladder Pancreatitis
Diagnosing gallbladder pancreatitis needs a few tests and imaging methods. Signs of inflammation and increased pancreatic enzyme levels can be detected through blood tests. CT scans, ultrasounds, or MRIs can find gallstones and see if there is any damage to the organs.
A correct diagnosis is important. It helps to confirm pancreatitis and plan the right treatment. The tools used are key for finding gallstone blockages and other issues. They play a crucial role in effectively handling the situation.
Common Diagnostic Tests

A simple way to check for pancreatitis of the gallbladder starts with blood tests.
- A lot of pancreatic enzymes means there is inflammation.
- Liver enzymes can show if there are blockages in the bile duct.
Imaging methods include:
- Ultrasound and CT scans are used to find gallstones or see if any organs are damaged.
- In tough cases, MRI might be used to get clearer pictures of any blockages.
These tests provide valuable information. This helps experts make a good treatment plan. Using these tests lets them act quickly to prevent serious complications.
Role of Imaging in Diagnosis
Imaging methods are important for detecting gallbladder pancreatitis. They provide clear pictures of any blockages in the ducts and the condition of the pancreas. Here is a list that compares different imaging tools:
- MRI: It shows clear images of the pancreatic ducts and any swelling around them.
- CT Scan: This scan provides cross-sectional images. It helps find damage to the pancreas and checks for blockages.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): This method combines imaging and treatment. It can remove gallstones directly.
These tools work together to provide good diagnostics. They help plan effective treatments for gallbladder and pancreatitis.
Treatment Options at Southlake General Surgery

At Southlake General Surgery, they provide treatment for gallbladder pancreatitis. This care includes simple options and more advanced choices. Dr. Valeria Simone, MD, develops personalized plans to help lessen symptoms and address the main issues.
She offers pain relief with medications and antibiotics. For some patients, she performs gallbladder removal through laparoscopic cholecystectomy or traditional surgery. Dr. Simone prioritizes personalized care to prevent future problems and improve their quality of life.
Initial Management Steps
Care for gallbladder pancreatitis begins with easing symptoms. Some critical things to think about are these:
- Pain Relief: Patients get medicine through an IV. This helps them feel more comfortable and reduces inflammation. In some cases, removal of the gallbladder may be necessary for long-term relief.
- Antibiotics: These medicines may be used to prevent or treat infections that can occur in severe pancreatitis.
- Intensive Care: In serious cases, patients might need to stay in an intensive care unit. Doctors monitor vital signs and provide IV fluids to help with dehydration.
The first step in treatment is very important. It helps make the patient’s condition stable. This step also prepares them for surgery later, if they need it.
Surgical Procedures by Dr. Simone
Dr. Simone develops different surgical options to remove the gallbladder and fix blocked ducts. The main choices are:
- Laparoscopic cholecystectomy: A safer option that helps people recover faster and has fewer risks.
- Traditional open surgery: This is necessary for severe inflammation or other serious issues, making sure that any dangerous blockages are taken out.
- Advanced techniques (like ERCP): These methods are used to assist in removing gallstones.
Dr. Simone pays attention to details. He provides safe and complete treatments. His work helps fix digestive problems. It also lowers the risk of future issues, like gallbladder pancreatitis.
Preventing Gallbladder Pancreatitis
Preventive steps for gallbladder pancreatitis focus on reducing the risk of gallstones and improving your digestive health. Key methods include changing your diet, managing your weight, and cutting down on alcohol.
Regular check-ups and healthcare are important to prevent issues. By managing risk factors, you can greatly lower your chance of having gallbladder pancreatitis.
Dietary and Lifestyle Adjustments
Eating healthy can help prevent gallstones. A low-fat diet with lots of fruits and vegetables can lower cholesterol levels in bile.
You should limit or stay away from alcohol. It can cause problems with your gallbladder. You can keep your weight in a healthy range by exercising regularly. It also helps your gallbladder work well.
Making these healthy changes can lower your chance of getting pancreatitis. This can help boost your digestion and improve your overall health.
Monitoring and Regular Check-Ups
Consistent evaluations with your healthcare professional hold significant value. They help to manage the risks of pancreatitis linked to the gallbladder. Some important things to consider are:
- Watching blood tests and medical images can help find gallstones quickly.
- A thorough check looks at how well your pancreas works and tells you about your digestion.
- Taking action fast can prevent serious problems, giving you peace of mind and keeping you well.
- Teaming up with a trusted healthcare provider helps prevent issues and reduces the risk of complications.
Conclusion
Gallbladder pancreatitis is a serious health problem that needs urgent attention and the right treatment. It is important to know the connection between gallstones and pancreatitis. Understanding this can help diagnose and treat the issue quickly.
Delays in care can lead to severe complications, such as pancreatic necrosis or permanent damage. Spotting symptoms early, like abdominal pain, jaundice, or nausea, can lead to emergency treatment and help prevent more issues, especially in people at higher risk.
Making changes to what you eat, drinking less alcohol, and going for regular check-ups can really lower your risk of inflammation of the pancreas.
If you experience this problem often, it’s important to talk to a healthcare provider about treatments like laparoscopic cholecystectomy. This can help your long-term health. Act now for your wellness by addressing this condition early.
Make an Appointment
If you experience symptoms of gallbladder pancreatitis, it is advisable to consult a healthcare professional. Dr. Valeria Simone, MD, at Southlake General Surgery, is ready to check your condition. She offers personal care for both acute and chronic pancreatitis.
To schedule an appointment, call +1 (817) 748-0200. At the office, you will undergo complete tests, like blood tests and CT scans, to discover the cause of pancreatitis. The team will also discuss treatments to help reduce your pain and improve your digestive health.
Frequently Asked Questions
What are the risk factors for developing gallbladder pancreatitis?
Risk factors for gallbladder pancreatitis are heavy alcohol use, a family history of gallstones, obesity, and health problems that raise cholesterol levels. Understanding the causes of pancreatitis can help you lower your risk. To lower your risk, you should manage your weight, keep track of your cholesterol, and reduce alcohol consumption.
Can gallbladder pancreatitis be completely cured?
Gallbladder pancreatitis can be treated well, often with surgery and care for the symptoms. However, chronic pancreatitis can cause permanent damage, and due to the associated risks, it can lead to a higher mortality rate. This damage requires ongoing care to handle complications and stop it from coming back.
How long is the recovery period after treatment?
Recovery time can change depending on how serious your condition is and what kind of surgery you have. For minimally invasive surgery, such as laparoscopic cholecystectomy, you usually need about two weeks to heal. But if you have traditional open surgery, recovery might take six to eight weeks after the procedure.
What dietary changes are recommended to prevent recurrence?
It is important to follow a low-fat diet. You should focus on healthy eating and avoid alcohol consumption. These changes can help lower the risk of gallstones. They can also reduce stress on digestion and lower the chance of gallstones returning.
How does Dr. Simone’s approach differ from typical treatments?
Dr. Simone creates treatment plans that fit each patient’s needs. She also works on new surgical methods. Her primary objective is to guarantee that her patients receive the care they need. This way, she can design unique solutions to reduce symptoms, tackle complications, and stop future problems quickly and carefully.
Medically Reviewed By: Dr. Valeria Simone MD
Board-certified General Surgeon at Southlake General Surgery, Texas, USA.
Follow us on Facebook and YouTube.
References:
- Mohy-Ud-Din, N., & Morrissey, S. (2023, July 4). Pancreatitis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK538337/
- Rashid, M. U., Hussain, I., Jehanzeb, S., Ullah, W., Ali, S., Jain, A. G., Khetpal, N., & Ahmad, S. (2019). Pancreatic necrosis: Complications and changing trend of treatment. World Journal of Gastrointestinal Surgery, 11(4), 198–217. https://doi.org/10.4240/wjgs.v11.i4.198
- Gapp, J., Tariq, A., & Chandra, S. (2023, February 9). Acute pancreatitis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK482468/
- Bartel, M. (2024, June 5). Acute pancreatitis. Merck Manual Consumer Version. https://www.merckmanuals.com/home/digestive-disorders/pancreatitis/acute-pancreatitis#v755288
- Pancreatitis – NIDDK. (n.d.-c). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/pancreatitis

