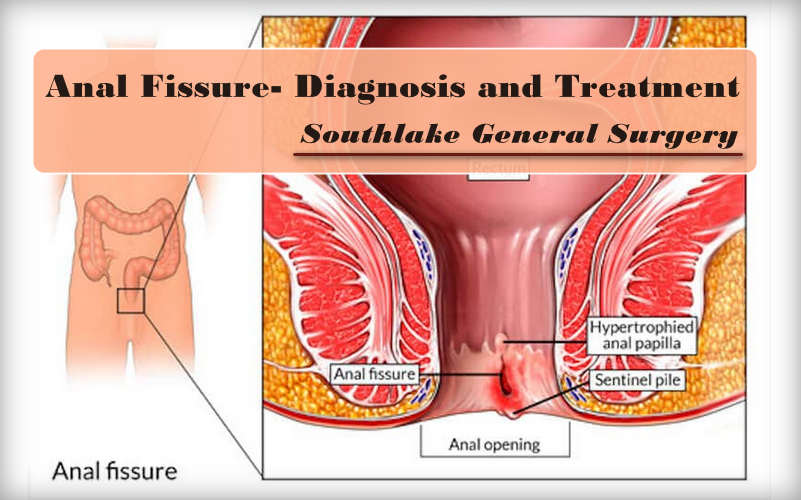
An anal fissure is a little cut or tear in the lining of the rear-end (anus). The crack in the skin create serious pain and some bleeding during and post bowel movements.
An anal fissure generally is not a severe condition. It can impact individuals of all age groups and it’s often found in babies and small kids since constipation is a typical issue in these age groups.
In many cases, the tear heals all alone within four to six weeks. In situations where the fissure continues past about two months, it’s viewed as chronic. On occasion, the fissure can be sufficiently profound to uncover the muscle tissue underneath.
Certain medicines can advance healing and help alleviate distress, including stool softeners and effective pain relievers.
If an anal fissure doesn’t improve with these medicines, you may require a surgery.
Symptoms of Anal Fissure
An anal fissure may cause at least one of the accompanying symptoms:
- a noticeable tear in the skin around anus
- itching and burning sensation around anal region
- strain of blood on stools or on toilet paper
- small bulge of skin, a skin tag, close to the tear
- sharp pain in the anal region during bowel movement
How do anal fissures occur?
An anal fissure mainly happens when passing enormous or hard stools. Chronic constipation or regular diarrhea can likewise tear the skin around anus. Other basic reasons include:
- excess straining during childbirth or bowel movements
- (IBD)-inflammatory bowel disease for example; Crohn’s disease
- decreased blood flow to the anorectal area
- reduced blood supply to the anorectal region
- excessively fitted or spastic anal sphincter muscles
In uncommon cases, an anal fissure may create due to:
- anal cancer
- tuberculosis
- herpes
- HIV
- syphilis
How do you at the risk of an anal fissures?
Anal fissures are usual during infancy. Old aged people are additionally inclined to anal fissures because of reduced blood supply in the anorectal region. During and after labor, women are at risk for anal fissures because of stressing during childbirth.
Individuals with IBD additionally have a higher risk for creating anal fissures. The irritation that happens in the intestinal lining form the tissue around the anus more inclined to tearing.
Individuals who often experience constipation are at an expanded risk for anal fissures also. Stressing and passing hard stools are the most well-known reasons for anal fissures.
How to diagnose an anal fissure?
A doctor can diagnose an anal fissure by examining the region of anus. However, they might need to prescribe for rectal test to affirm the diagnosis.
During this test, the medical specialist may embed an anoscope into rectum to make it simpler to see the tear. This medical equipment is a slim tube that help specialists to examine the anal canal.
With the help of an anoscope doctor can locate other reasons for anal or rectal pain, for example, hemorrhoids. In few cases of rectal pain, you may require an endoscopy for better assessment of symptoms.
Treatment of an anal fissure
Many anal fissures don’t need broad treatment. Certain home remedies can help advance healing and ease painful symptoms. Home treatment for anal fissure include:
- using over-the-counter stool softeners
- using Stool softeners
- drink plenty of fluids
- High fiber meal such as green salads and fresh fruits
- regular sitz bath to ease the anal muscles, relieve inflammation and strengthen blood flow to the anorectal region
- application of ointment to increase blood flow to the affected area to help ease inflammation
If your side effects aren’t diminished within two weeks of treatment, consult with your PCP for additional assessment. Your PCP can ensure you have the right diagnosis and can suggest different medicines.
A calcium channel blocker ointment can loosen up the sphincter muscles and permit the anal fissure to recuperate.
There is another preferred treatment is Botox infusions into the anal sphincter. The injections will forestall spasms in anus by provisionally paralyzing the muscle. This permits anal fissure to heal while keeping new fissures from shaping.
If your anal fissure neglects to react to other medicines, your primary care physician may suggest an anal fissure sphincterotomy. This surgery includes making a small cut in the anal sphincter to loosen up the muscle. Loosening up the muscle permits the anal fissure to recuperate.
Not all anal fissures are an indication of low-fiber diets and constipation. Ineffectively healing fissures or those situated in a position other than the back and midline portion of anus may show an underlying condition.
If you have any worries about a fissure that is not recuperating even attempting at-home remedies, consult with your PCP to check whether you need any extra examinations.
How to prevent an anal fissure?
An anal fissure can’t generally be forestalled; however, you can lessen risk of getting one by taking the accompanying preventive measures:
- always keep the anal region dry
- cleansing the anal region gently with mild cleanser and Lukewarm water
- drinking plenty of liquids, eating high-fiber meals, and regular workout to avoid constipation
- Treating diarrhea right away
- changing babies’ diapers immediately
Conclusion
Anal fissures may create sharp pain and modest amount of red blood with bowel movement. If it turns into a chronic anal fissure, skin tags may create in the region related with a chronic local infection.
Conditions related with anal fissures incorporate past anal surgical procedures, irritating bowel disease, tumors, and sexually transmitted diseases.
A few conditions that may even more straightforwardly lead to anal fissures are ones that prompt injury to the region, for example, vaginal delivery, anal sex, or passing hard stool. For more information on Anal Fissure and consultation. Contact our healthcare expert at +1 817-748-0200 or Click Here to Book an Online Appointment with us.