Epigastric hernia surgery may be necessary if the hernia is causing symptoms such as pain, discomfort, or difficulty with daily activities. The type of surgery recommended will depend on the size and location of the hernia, as well as the patient’s overall health.
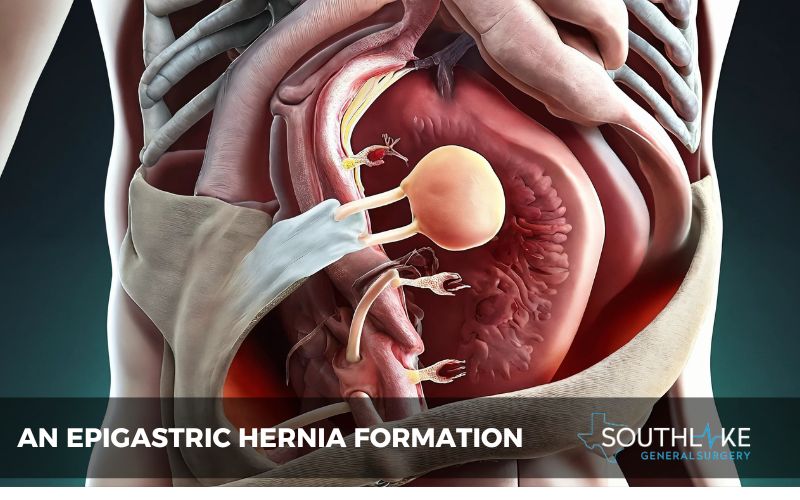
Epigastric hernia is a common type of hernia that occurs in the upper abdomen, between the belly button and sternum. They occur when there is a weakness in the abdominal wall, allowing fat to push through and form a bump or lump.
While epigastric hernias can be relatively small and asymptomatic, they can also cause pain, tenderness, and discomfort.
Understanding what causes epigastric hernias, their symptoms, and treatment is crucial for those at risk. This blog offers a detailed look into diagnosis, treatment choices, and recovery from epigastric hernias.
By understanding the different aspects of epigastric hernias, individuals can make informed decisions about their treatment options and recovery process. Whether you are seeking non-surgical treatment options or considering surgery, the information in this blog will help you navigate your journey toward better health and well-being.
Key Highlights
- An epigastric hernia is a type of hernia that occurs in the upper abdomen, between the belly button and sternum.
- A weak belly wall that allows fat to push through and form a lump is the cause of an epigastric hernia.
- Symptoms of an epigastric hernia include pain, tenderness, and a visible lump in the affected area.
- Diagnosing an epigastric hernia can be done through physical examination and imaging tests.
- Treatment options for epigastric hernia include both non-surgical and surgical approaches.
- Non-surgical treatments may include lifestyle changes, such as weight loss and avoiding activities that worsen symptoms.
- Surgical options for epigastric hernia repair include laparoscopic surgery and open hernia repair.
- Recovery after epigastric hernia surgery varies, but most people can return to normal activities within a few weeks.
- Life after hernia surgery may require some lifestyle adjustments, such as maintaining a healthy weight and regular follow-up care.
Understanding Epigastric Hernias

Epigastric hernias occur in the epigastric region, also known as the epigastrium, which is the area between the belly button and sternum. The abdominal wall, which is made up of four layers, protects the organs in the abdominal cavity, including the intestines.
A weakness in the abdominal wall can allow fat to push through and form a lump in the upper abdomen. This lump is characteristic of an epigastric hernia and can cause pain and discomfort.
What Is an Epigastric Hernia?
An epigastric hernia is a specific type of hernia that occurs in the upper abdomen, between the belly button and sternum. It is characterized by a weakness in the abdominal wall, allowing fat to push through and form a lump.
This weakness can be caused by various factors, including a congenital defect or repetitive strain on the abdominal muscles. Epigastric hernia is a common type of abdominal hernia, making up about 2 to 3 percent of all cases. They can occur in both adults and children and are often seen in infants.
The most common location for an epigastric hernia is along the midline of the abdomen, where the abdominal muscles meet. This area, known as the Linea alba, is a weak spot where the abdominal wall is thinner. When fat pushes through this weak spot, it forms a visible lump that can range in size and cause discomfort.
Causes and Symptoms of Epigastric Hernias
There are numerous causes of epigastric hernias, including:
- Weakness in the abdominal wall from birth
- Repetitive strain on abdominal muscles
- Abdominal pain or discomfort is the most typical symptom of an epigastric hernia, and activities like lifting heavy objects can make it worse.
- Other symptoms may include tenderness or a visible lump in the upper abdomen.
- Risk factors for developing an epigastric hernia include obesity, smoking, and a family history of hernias.
Recognizing these risk factors and symptoms is crucial for early diagnosis and treatment.
Diagnosing Epigastric Hernias
Diagnosing an epigastric hernia typically involves a combination of physical examination and imaging tests. During a physical examination, a healthcare professional may feel for a lump or bulge in the upper abdomen and ask about symptoms, such as pain or discomfort.
Imaging tests, such as ultrasound or CT scan, may be used to confirm the presence and location of the hernia. These tests can provide detailed images of the abdominal area, allowing healthcare professionals to assess the size and severity of the hernia. Once a diagnosis is made, appropriate treatment options can be discussed and explored.
Common Diagnostic Tests
When diagnosing an epigastric hernia, healthcare professionals may use a variety of diagnostic tests. These tests can help confirm the presence of a hernia and provide detailed information about its size and location.
- One common diagnostic test is an ultrasound, which uses sound waves to create images of the abdominal area. This can help healthcare professionals visualize the hernia and determine its characteristics.
- Another common test is a CT scan, which uses X-rays and computer technology to create detailed cross-sectional images of the abdomen. This can provide a more comprehensive view of the hernia and surrounding tissues.
- In some cases, surgical exploration may be necessary to confirm the presence of a hernia and assess its size and location. This may involve making a small incision in the abdominal wall to directly visualize the hernia.
By using these diagnostic tests, healthcare professionals can accurately diagnose an epigastric hernia and develop an appropriate treatment plan.
When to See a Doctor
- Seek medical attention if you suspect you may have an epigastric hernia or are experiencing symptoms such as abdominal pain, discomfort, or a visible lump in the upper abdomen.
- Not all hernias require immediate medical intervention, but it’s crucial to have any symptoms evaluated by a healthcare professional to rule out serious complications.
- Consult with a healthcare professional, even if your symptoms are minor or do not interfere with your daily activities for a proper diagnosis and guidance on treatment options.
Early detection and intervention can help prevent hernia progression and minimize the risk of complications.
Treatment Options for Epigastric Hernias
The treatment options for epigastric hernias depend on the size and severity of the hernia, as well as the presence of symptoms. In some cases, non-surgical treatments may be recommended, while in other cases, surgical intervention may be necessary.
Non-surgical treatments for epigastric hernias may include lifestyle modifications, such as avoiding activities that worsen symptoms and maintaining a healthy weight. These measures can help alleviate discomfort and reduce the risk of complications.
Surgical options for epigastric hernia repair include laparoscopic surgery and open hernia repair. The selection of the surgical method is based on several factors, such as the hernia’s size and placement, along with the person’s general health condition.
Non-Surgical Treatments and Their Effectiveness
Non-surgical treatments for epigastric hernias focus on managing symptoms and reducing the risk of complications.
Lifestyle modifications, such as avoiding activities that worsen symptoms and maintaining a healthy weight, can help alleviate discomfort and reduce the risk of hernia enlargement. Losing weight can relieve pressure on the abdominal wall, reducing the risk of the hernia worsening.
Additionally, individuals with acid reflux or gastroesophageal reflux disease (GERD) may benefit from dietary changes and the use of medications to reduce stomach acid production. This can help prevent acid reflux symptoms, which can worsen hernia-related discomfort.
While non-surgical treatments may provide symptomatic relief, they may not address the underlying cause of the hernia. In cases where symptoms persist or the hernia becomes larger or more painful, surgical intervention may be necessary to repair the hernia.
Overview of Surgical Options
Surgical intervention is often necessary to repair an epigastric hernia, especially in cases where symptoms persist, or the hernia becomes larger or more painful.
The two main surgical options for epigastric hernia repair are laparoscopic surgery and open hernia repair. Various factors, such as the hernia’s size and location and the individual’s overall health, influence the selection of the surgical approach.
- Laparoscopic surgery involves making small incisions in the abdomen and using specialized instruments and a camera to repair the hernia. This approach offers the advantages of less post-operative pain, shorter recovery time, and smaller scars.
- Open hernia repair involves making a larger incision directly over the hernia and repairing the abdominal wall. This approach may be necessary in cases where the hernia is large or complex.
Both surgical options are typically performed under general anesthesia, and the choice of approach is based on the individual’s specific circumstances and the surgeon’s expertise.
Preparing for Epigastric Hernia Surgery

Preparing for epigastric hernia surgery involves several steps to ensure a successful procedure and optimal recovery.
If you smoke, quitting smoking prior to surgery is highly recommended, as it can reduce the risk of complications and improve overall health. Maintaining a healthy weight and engaging in regular exercise can also help prepare the body for surgery and aid in post-operative recovery.
It is important to follow any pre-operative instructions provided by the healthcare team, such as fasting before surgery and avoiding certain medications that may interfere with the procedure.
By taking these steps to prepare for surgery, individuals can help minimize the risk of complications and ensure a smooth recovery process.
Understanding the Risks and Complications
Like any surgical procedure, epigastric hernia surgery carries certain risks and potential complications. It is important to understand these risks and discuss them with your healthcare team before undergoing surgery.
Some general complications that can occur with any surgical procedure include bleeding, infection of the surgical site, allergic reactions to anesthesia or medications, and blood clots. These risks can be minimized by following pre-operative instructions and taking the necessary precautions.
Specific complications associated with epigastric hernia surgery may include the development of a collection of blood or fluid under the wound, injury to structures within the abdomen, and unsightly scarring of the skin. Your surgeon will talk to you about these risks and work to reduce the chances of them happening.
It is important to remember that while these risks exist, the majority of epigastric hernia surgeries are successful and result in a smooth recovery.
The Surgical Procedure Explained
The surgical procedure for repairing an epigastric hernia involves several steps to address the hernia and reinforce the abdominal wall.
Under general anesthesia, your surgeon will make an incision over the hernia site and free up the hernial sac. If only fat is pushing through the hernia, your surgeon may remove the fat or push it back using a general anesthetic. If abdominal contents are also pushing through, they will be placed back inside the abdomen.
The hernial sac will then be removed, and the weak spot in the abdominal wall will be closed with sutures or a synthetic mesh. This reinforcement helps strengthen the abdominal wall and prevent future hernias from developing.
The procedure typically takes about 30 minutes, but the exact time can vary depending on the individual case and the surgical technique used.
What Happens During Surgery
During epigastric hernia surgery, several steps are taken to repair the hernia and strengthen the abdominal wall.
Under general anesthesia, your surgeon will make an incision over the hernia site and carefully free up the hernial sac. If only fat is pushing through the hernia, your surgeon may remove the fat or push it back into the abdominal cavity. If abdominal contents, such as intestines, are also pushing through, they will be gently placed back inside the abdomen.
The hernial sac will be removed, and the weak spot in the abdominal wall will be closed with strong sutures or a synthetic mesh. This closure helps reinforce the abdominal wall and prevent future hernias from developing.
Sutures or surgical staples will be used to close the incision, followed by the application of a sterile dressing to the surgical site.
Recovery After Epigastric Hernia Surgery
Recovery after epigastric hernia surgery varies for each individual but typically involves a period of rest and a gradual return to normal activities.
The majority of individuals can be discharged on the day of the surgery, but a few might require an overnight stay for monitoring purposes. Pain relief medication might be recommended to help control any pain experienced throughout the healing process.
It is important to follow your surgeon’s instructions for post-operative care, which may include avoiding heavy lifting or strenuous activities for several weeks. Gradually increasing physical activity and returning to normal activities as tolerated is recommended.
Most people can resume normal activities within a few weeks, although it may take several months for a full recovery.
Immediate Post-Surgery Care

After epigastric hernia surgery, it is important to take proper care of the surgical site to promote healing and minimize discomfort.
You may experience some pain and discomfort at the surgical site, which can be managed with prescribed pain medication. Your surgeon may also recommend icing the area to reduce swelling.
Maintaining cleanliness and dryness at the surgical site is equally important. You will be instructed on how to care for the wound and when it is safe to shower or bathe.
You may also be advised to wear a supportive abdominal binder or a compression garment to provide additional support and reduce swelling.
Follow-up appointments with your surgeon will be scheduled to monitor your healing progress and address any concerns or complications that may arise.
Long-Term Recovery Tips
To support long-term recovery after epigastric hernia surgery, it is important to maintain a healthy lifestyle and follow any recommendations provided by your healthcare team.
Maintaining a healthy weight through regular exercise and a balanced diet can help prevent hernia recurrence and promote overall well-being.
Engaging in regular physical activity, as tolerated, can help strengthen the abdominal muscles and aid in recovery.
Be sure to follow any restrictions or guidelines provided by your surgeon regarding lifting heavy objects or participating in strenuous activities. Gradually increasing physical activity and returning to normal activities as tolerated is recommended.
Attending scheduled follow-up appointments with your surgeon is important to monitor your recovery progress and address any concerns or complications that may arise.
Life After Hernia Surgery

Life after hernia surgery may require some adjustments to ensure long-term health and prevent future hernias.
Maintaining a healthy lifestyle, including regular exercise and a balanced diet, can help prevent hernia recurrence and promote overall well-being.
Engaging in activities that promote good posture and proper body mechanics can also help reduce the risk of future hernias.
Follow-up care, including regular check-ups with your surgeon and any necessary imaging or diagnostic tests, is important to monitor your recovery progress and detect any potential complications.
Your healthcare team will provide guidance and support throughout your recovery journey, helping you navigate the necessary lifestyle changes and follow-up care to maintain optimal health.
Adjusting Your Lifestyle for Better Health
Making lifestyle adjustments can help improve your overall health and reduce the risk of hernia recurrence.
Maintaining a healthy weight through regular exercise and a balanced diet is important for preventing hernias and promoting overall well-being. Obesity is a risk factor for developing hernias, so achieving and maintaining a healthy weight is essential.
Quitting smoking is also important, as smoking can impair the healing process and increase the risk of complications. Smoking can also weaken the abdominal muscles, making it more likely for hernias to occur or recur.
By making these lifestyle adjustments, you can support your long-term health and reduce the risk of future hernias.
Follow-Up Care and Monitoring

Follow-up care and monitoring are important aspects of long-term hernia management.
Your healthcare team will schedule regular follow-up appointments to monitor your recovery progress and assess for any potential complications or recurrent hernias. These appointments may include physical examinations, imaging tests, and discussions about any ongoing symptoms or concerns.
Monitoring may also include lifestyle assessments, such as assessing your weight, activity level, and overall health. Your healthcare team may provide guidance and support for maintaining a healthy lifestyle and preventing future hernias.
By staying engaged with your healthcare team and attending scheduled follow-up appointments, you can ensure that your hernia is properly managed and any potential issues are addressed promptly.
Outlook
The outlook for individuals with epigastric hernias is generally positive, especially with appropriate treatment and follow-up care.
With surgical intervention, most people can expect a successful repair and a smooth recovery. The risk of hernia recurrence can vary depending on factors such as the size and location of the hernia, as well as an individual’s overall health and lifestyle choices.
By maintaining a healthy lifestyle, following post-operative instructions, and attending scheduled follow-up appointments, individuals can help minimize the risk of recurrence and optimize their long-term prognosis.
Make An Appointment

If you are experiencing symptoms of an epigastric hernia or have been diagnosed with one and would like to explore treatment options, it is recommended to make an appointment with a qualified healthcare provider.
Dr. Valeria Simone MD, at Southlake General Surgery in Texas, USA, specializes in hernia repair and can provide expert care and guidance. To schedule an appointment, please call +1 (817) 748-0200.
Dr. Simone, and her team are committed to providing excellent care and helping individuals achieve optimal health and well-being.
Frequently Asked Questions
Can Epigastric Hernias Reoccur After Surgery?
Yes, epigastric hernias can reoccur after surgery. The risk of recurrence depends on various factors, including the size and location of the hernia, the condition of the abdominal wall, and individual risk factors. However, with appropriate surgical techniques and lifestyle modifications, the risk of recurrence can be minimized.
How Long Is the Recovery Period?
The recovery period after epigastric hernia surgery can vary depending on the individual and the surgical approach used. Most people can return to normal activities within a few weeks, but it may take several months for a full recovery. It is important to follow your surgeon’s instructions and gradually increase physical activity to allow for proper healing of the abdominal muscles.
Are There Diet Restrictions Post-Surgery?
Your surgeon may recommend certain diet restrictions following epigastric hernia surgery. This may include avoiding spicy or acidic foods that can increase stomach acid production and cause discomfort. It is important to follow your surgeon’s recommendations to support proper healing and minimize digestive symptoms.
What Are the Signs of Complications to Watch For?
After epigastric hernia surgery, it is important to watch for signs of complications, such as infection, excessive abdominal pain, nausea, vomiting, or difficulty urinating. These symptoms should be reported to your healthcare team immediately for further evaluation and appropriate treatment.
Medically Reviewed By: Dr. Valeria Simone MD
Board-certified General Surgeon at Southlake General Surgery, Texas, USA.
Follow us on Facebook and YouTube.
References:
- Vemulakonda SHP, Dutta S, Jain A, Reddy A, Nelamangala Ramakrishnaiah VP. Strangulated Epigastric Hernia: A Rare Occurrence. Cureus. 2021;13(3):e14038. Published 2021 Mar 22. https://doi:10.7759/cureus.14038
- Pegoli, Walter, and George T. Drugas. “Hernias, Abdominal Wall.” Elsevier eBooks, vol. 264–265, 1 Jan. 2007, https://doi.org/10.1016/b978-032303506-4.10148-8.
- Mehta H. Abdominal Pain. Clinical Pathways in Emergency Medicine. 2016;329-345. Published 2016 Feb 22. https://doi:10.1007/978-81-322-2710-6_26
- Ponten, J. E. H., et al. “Pathogenesis of the Epigastric Hernia.” Hernia, vol. 627–633, no. 6, 24 July 2012, https://doi.org/10.1007/s10029-012-0964-8.
- “[Diagnosis and Treatment of Epigastric Hernia. Analysis of Our Experience].” PubMed, 1 Sept. 2000, www.ncbi.nlm.nih.gov/pubmed/11155474.
- Blonk L, Civil YA, Kaufmann R, Ket JCF, van der Velde S. A systematic review on surgical treatment of primary epigastric hernias. Hernia. 2019;23(5):847-857. https://doi:10.1007/s10029-019-02017-4
- Robinson, Patrick, and John C. Perkins. “Approach to Patients With Epigastric Pain.” Emergency Medicine Clinics of North America, vol. 191–210, no. 2, 1 May 2016, https://doi.org/10.1016/j.emc.2015.12.012.

