Hemorrhoidectomy is a surgical procedure performed to remove hemorrhoids that have not responded to other treatments or have caused serious complications. It is often recommended when hemorrhoids have prolapsed, thrombosed (developed a blood clot), or become strangulated (blood supply cut off).
During a hemorrhoidectomy, the affected hemorrhoidal tissue is excised, and the blood vessels are sealed to promote healing. The procedure can provide long-term relief from hemorrhoid symptoms and prevent recurrence.
While hemorrhoidectomy is an effective treatment option, it is important to understand the risks and the recovery process associated with the procedure.
Hemorrhoids, also known as piles, are swollen blood vessels in the anal canal and rectum. They can be internal, located inside the rectum, or external, located under the skin around the anus. Hemorrhoids can cause discomfort, pain, itching, and bleeding.
While most cases of hemorrhoids can be managed with conservative treatments such as dietary changes, lifestyle modifications, and over-the-counter medications, there are instances where surgical intervention may be necessary.
This blog will provide an overview of hemorrhoidectomy, including when it may be necessary, the different types of procedures, the recovery and aftercare, and the potential risks and complications. It will also highlight the approach of Dr. Valeria Simone at Southlake General Surgery and the benefits of choosing their healthcare services for hemorrhoidectomy.
Key Highlights
- Both internal and external hemorrhoids can be surgically removed through a hemorrhoidectomy surgery.
- It is often recommended when other treatments have failed or when there are complications such as prolapse, thrombosis, or strangulation.
- The procedure involves cutting out the affected hemorrhoidal tissue and sealing the blood vessels.
- Recovery time can vary, but most people can expect to see an improvement within two to four weeks.
- Pain management, sitz baths, and stool softeners are important aspects of the recovery process.
- Hemorrhoidectomy has a high success rate and provides long-term relief from hemorrhoid symptoms.
Understanding Hemorrhoids and the Need for Surgery
Hemorrhoids, whether internal or external, can cause discomfort in the anal area due to swollen blood vessels. When less invasive treatments fail to provide relief, surgical options like hemorrhoidectomy become necessary.
Signs indicating the need for surgery include severe bleeding, prolapse, or thrombosis. Understanding the nature of hemorrhoids and the potential need for surgical intervention is crucial in managing this condition effectively.
What Are Hemorrhoids?
Hemorrhoids are enlarged blood vessels located in the rectum or anus, which can result in discomfort and bleeding. They can be internal or external and are common due to straining during bowel movements. Hemorrhoids may require surgical removal if conservative treatments fail.
Signs That You May Need Surgical Intervention

If you experience severe pain, excessive bleeding, or prolapsed hemorrhoids that do not retract on their own, surgical intervention such as a hemorrhoidectomy may be necessary.
Other indications include recurrent hemorrhoids that do not respond to non-invasive treatments like sitz baths or over-the-counter remedies. It’s crucial to consult with a healthcare provider if you notice persistent symptoms despite conservative measures.
Seeking timely medical advice can help address potential complications and provide relief from discomfort.
Dr. Valeria Simone’s Approach to Hemorrhoidectomy
Dr. Valeria Simone prioritizes patient care and precision in performing hemorrhoidectomies. With a focus on utilizing advanced surgical techniques for optimal outcomes, Dr. Simone ensures thorough pre-surgery consultations to address individual needs.
At Southlake General Surgery, patients benefit from her expertise in both traditional and innovative hemorrhoidectomy procedures. Dr. Simone’s approach emphasizes patient comfort and safety throughout the surgical process. Her dedication to delivering exceptional results makes her a trusted choice for hemorrhoid surgery.
Why Choose Southlake General Surgery?
When opting for hemorrhoidectomy, Southlake General Surgery stands out for its specialized care and expertise. With a focus on patient well-being and successful outcomes, their team ensures personalized attention and top-notch surgical techniques.
The Pre-Surgery Consultation Process
During the pre-surgery consultation process, your health information and specific details about your hemorrhoids will be thoroughly reviewed. Your healthcare provider will discuss the type of surgery required based on the severity of your condition.
They will also provide instructions on preparing for the procedure, which may include avoiding certain medications like blood thinners.
This consultation ensures that you are well informed about the upcoming surgery and are ready both physically and mentally for the hemorrhoidectomy procedure.
Types of Hemorrhoidectomy Procedures
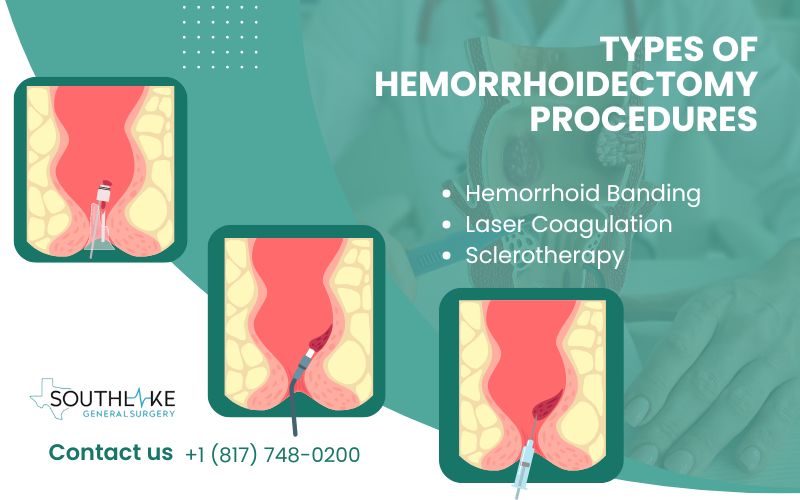
Surgical removal of hemorrhoidal tissue is the standard procedure for hemorrhoidectomy. Another method is hemorrhoid banding, where a rubber band is used to cut off the blood supply to the hemorrhoid.
Advanced techniques like laser coagulation or infrared light can treat hemorrhoids non-surgically. A closed hemorrhoidectomy involves wound closure post-procedure, while an open hemorrhoidectomy leaves the wound open.
Your surgeon will recommend the most suitable type based on your condition and factors like recovery time and postoperative discomfort.
Traditional Hemorrhoidectomy Explained
Traditional hemorrhoidectomy involves surgically removing hemorrhoids using a scalpel. Under general anesthesia, this operation is usually carried out.
During the surgery, the hemorrhoidal tissue is excised, and the wound is closed using sutures. Recovery time can vary, but patients may experience postoperative pain.
Stool softeners and pain medications are usually prescribed to manage discomfort. It is essential to follow postoperative care instructions diligently for optimal healing and to minimize the risk of complications.
Advanced Surgical Techniques for Hemorrhoid Removal
Advanced surgical techniques for hemorrhoid removal involve innovative procedures like hemorrhoidopexy and sclerotherapy.
- Hemorrhoidopexy lifts and fixes prolapsed hemorrhoids back to their normal position, reducing discomfort and prolapse.
- Sclerotherapy involves injecting a solution to shrink hemorrhoids.
These methods offer less postoperative pain and faster recovery compared to traditional options, making them appealing choices for patients seeking effective and efficient hemorrhoid removal treatments.
Preparing for Your Hemorrhoid Surgery
Prior to your hemorrhoidectomy, it is essential to follow your doctor’s pre-surgery instructions diligently. Steps may include adjusting your diet to include more fiber, staying hydrated, and possibly using stool softeners.
Your healthcare provider may advise stopping certain medications, like blood thinners. Ensure all necessary arrangements are made for transportation post-surgery.
Understanding and adhering to these guidelines can help facilitate a smoother surgical experience and aid in your recovery.
Steps to Take Before Your Procedure
- Ensure to inform your surgeon of any blood thinners you may be taking and follow their guidance on their usage.
- Keep yourself hydrated by drinking plenty of water and try to maintain a healthy diet rich in fiber.
- Consult with your healthcare provider regarding the adjustment of any prescription medicine and inform them about any supplements you are taking.
- Additionally, remember to prepare your home environment for a comfortable recovery post-surgery.
What to Anticipate on the Day of Surgery

On the day of your hemorrhoidectomy surgery, expect to arrive at the hospital or surgical center early in the morning. Prior to the procedure, fasting will be necessary. Once admitted, you will change into a hospital gown and be prepared for the operation.
An anesthesiologist will discuss the type of anesthesia you will receive — either local, regional, or general anesthesia. Before the surgery, your surgeon will also explain the details of the procedure and answer any last-minute questions you might have.
The Hemorrhoidectomy Procedure

During a hemorrhoidectomy procedure, the surgeon removes hemorrhoidal tissue, offering relief from painful symptoms. This surgery can be done under general anesthesia or local anesthesia with sedation.
The process usually involves cutting out excessive tissue from the anal area. Depending on the severity, healthcare providers may opt for open or closed hemorrhoidectomy.
With advancements like infrared light or scalpel-free techniques, patients can experience less postoperative pain and a faster recovery time. This surgical intervention aims to address uncomfortable symptoms and improve the patient’s quality of life.
An Overview of the Surgical Process
During a hemorrhoidectomy, the surgeon carefully removes hemorrhoidal tissue located in the anal canal. The procedure can address both internal and external hemorrhoids, improving symptoms like bleeding or discomfort.
Surgical techniques may involve using a scalpel, a laser, or infrared light to treat the affected area. Prior to surgery, patients are likely to receive local or general anesthesia for pain management.
Wound closure methods vary depending on the type of surgery, with options including open or closed hemorrhoidectomy procedures. Postoperatively, patients are advised on recovery steps and potential complications.
Pain Management and Anesthesia Options
Pain management and anesthesia options are crucial aspects of a hemorrhoidectomy. Patients undergoing this procedure can typically choose between local anesthesia, spinal block, or general anesthesia based on their needs and the complexity of the surgery.
These options ensure that the patient remains comfortable throughout the operation and experiences minimal discomfort. Discuss with your healthcare provider to determine the most suitable option for your procedure. Effective pain management is essential for a smooth recovery process post-surgery.
Recovery and Aftercare Following Hemorrhoidectomy
After a hemorrhoidectomy, recovery and aftercare are crucial for a smooth healing process. You may experience some discomfort and pain post-surgery, which can be managed with prescribed pain medication.
It is advisable to consume stool softeners, stay hydrated, and maintain a high-fiber diet to avoid constipation. Engage in light physical activities and avoid heavy lifting to aid the recovery process.
Following hygiene practices like using gentle wipes or taking sitz baths can promote healing and reduce the risk of infection. Contact your healthcare provider immediately if you notice excessive bleeding, severe pain, or any concerning symptoms during your recovery period.
Immediate Post-Surgery Care
Following a hemorrhoidectomy, immediate post-surgery care plays a crucial role in recovery. Patients should expect some discomfort in the anal area, which can be managed with prescribed pain medication.
Adhering to a soft diet, including plenty of water and fiber-rich foods, aids in smoother bowel movements. Avoiding heavy lifting and straining during bowel movements is vital to prevent stress on the surgical site.
Additionally, maintaining hygiene through gentle cleansing with baby wipes instead of toilet paper can promote healing and reduce irritation.
Long-Term Healing and Recovery Tips
After undergoing a hemorrhoidectomy, focus on long-term care for efficient healing.
- Stay hydrated by drinking plenty of water to aid digestion and bowel movements.
- Consume a fiber-rich diet to prevent constipation, a common post-surgery issue.
- Regular exercise can promote healthy blood flow and reduce the risk of future hemorrhoids.
- Do not lift large objects or strain while you are doing bowel movements.
- Implement healthy habits, like using baby wipes instead of rough toilet paper.
- Monitor any discomfort or itching and consult your healthcare provider promptly if any concerns arise.
- Regular follow-ups ensure optimal recovery.
Potential Risks and Complications
Potential risks and complications associated with hemorrhoidectomy include bleeding, infection, and difficulty in controlling bowel movements.
In rare cases, serious complications such as fecal incontinence or damage to the anal canal’s muscles, may occur. It’s important to follow post-operative care instructions diligently to minimize these risks.
Consulting with your healthcare provider about potential complications and how to mitigate them is crucial for a successful recovery.
Common Post-Surgical Concerns
Post-surgical concerns following a hemorrhoidectomy may include bleeding, pain, or infection. It’s common to experience discomfort during bowel movements or when sitting.
Swelling and bruising in the anal area are normal postoperative symptoms. To alleviate these issues, follow your healthcare provider’s instructions diligently.
If you notice excessive bleeding or severe pain, contact your doctor immediately. It’s important to monitor your recovery carefully and seek medical advice for any unexpected developments. Stay informed about potential risks and complications for a smoother healing process.
How to Mitigate Risks After Hemorrhoid Surgery
After undergoing hemorrhoid surgery, it’s crucial to mitigate risks for a smooth recovery. Follow your healthcare provider’s instructions diligently. To reduce complications, avoid heavy lifting, and ensure you stay hydrated.
Implement a high-fiber diet to prevent constipation and follow recommended post-operative care practices. Take prescribed medications as directed and refrain from using blood thinners unless approved.
Pay attention to any unusual symptoms and contact your healthcare provider promptly if concerns arise. Adhering to these guidelines can help minimize potential risks post-hemorrhoid surgery.
Conclusion
If you are considering a hemorrhoidectomy, understanding the procedure and aftercare is crucial. Dr. Valeria Simone and Southlake General Surgery offer expert care and various surgical techniques for hemorrhoid removal.
From pre-surgery consultations to recovery tips, they prioritize your well-being. Be informed about potential risks, post-surgical concerns, and long-term healing.
If you have questions or need to schedule a consultation, don’t hesitate to get in touch. Your comfort and health are their priorities. Trust in their experience for a successful hemorrhoidectomy journey.
Make an Appointment
To schedule a consultation or make an appointment for a hemorrhoidectomy, contact our healthcare expert today at +1 (817) 748-0200.
Our team, led by Dr. Valeria Simone, specializes in the surgical removal of hemorrhoids using advanced techniques. Seeking prompt medical attention is crucial if you are experiencing persistent symptoms that may necessitate surgical intervention.
Don’t hesitate to reach out for personalized care and information regarding hemorrhoid surgery. Make your health a priority and take the first step towards relief.
Frequently Asked Questions
Is Hemorrhoidectomy the Best Option for Me?
Hemorrhoidectomy is considered when conservative treatments fail. Consult a specialist to assess if surgery is the best option based on your condition’s severity and impact on quality of life. Understanding the procedure and potential risks will help you make an informed decision.
How Long Is the Recovery Period?
Recovery time post-hemorrhoidectomy varies. Immediate care is crucial, with gradual improvement over 2–6 weeks. Factors like procedure type and individual healing affect the duration. Following surgeon guidelines aids in a smoother recovery process.
What Are the Alternatives to Hemorrhoidectomy?
While hemorrhoidectomy is a common surgical option, alternatives include non-surgical treatments like rubber band ligation, sclerotherapy, and infrared coagulation. These methods are less invasive and can be effective for managing hemorrhoids.
Can Hemorrhoids Recur After Surgery?
Hemorrhoids can recur after surgery if the underlying causes aren’t addressed. Factors like diet, lifestyle, and bowel habits play a role. Follow post-op care instructions diligently to reduce recurrence chances. Regular check-ups can help monitor and manage any reoccurrences effectively.
Medically Reviewed By: Dr. Valeria Simone MD
Board-certified General Surgeon at Southlake General Surgery, Texas, USA.
Follow us on Facebook and YouTube.
References:
- “Definition &Amp;Amp; Facts of Hemorrhoids.” National Institute of Diabetes and Digestive and Kidney Diseases, 23 July 2022, https://www.niddk.nih.gov/health-information/digestive-diseases/hemorrhoids/definition-facts
- “Treatment of Hemorrhoids.” National Institute of Diabetes and Digestive and Kidney Diseases, 23 July 2022, https://www.niddk.nih.gov/health-information/digestive-diseases/hemorrhoids/treatment
- “Hemorrhoids.” National Institute of Diabetes and Digestive and Kidney Diseases, 3 Mar. 2023, https://www.niddk.nih.gov/health-information/digestive-diseases/hemorrhoids/all-content
- Yeo D, Tan KY. Hemorrhoidectomy – making sense of the surgical options. World J Gastroenterol. 2014;20(45):16976-16983. https://doi:10.3748/wjg.v20.i45.16976
- Diurni, Mario, and Matteo Di Giuseppe. “Hemorrhoidectomy in Day Surgery.” International Journal of Surgery, vol. S53–S55, 1 Jan. 2008, https://doi.org/10.1016/j.ijsu.2008.12.018
- Cristea, Cosmina, and Catherine R. Lewis. “Hemorrhoidectomy.” StatPearls – NCBI Bookshelf, 3 July 2023, www.ncbi.nlm.nih.gov/books/NBK549864.
Cristea C, Lewis CR. Hemorrhoidectomy. 2023 Jul 3. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 31751054.