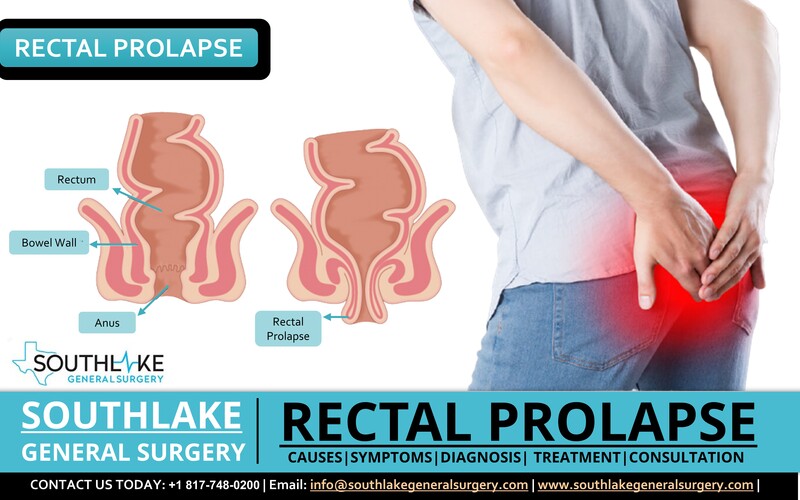
Rectal Prolapse happens when the rectum (the last part of the large intestines) slips out of the anus. It is a rare medical emergency and may create discomfort. It can happen at any age among men and women. If an individual ignores this condition for a long time, it may get worse with time.
You may not feel comfortable while passing stools and one should not ignore it. Consult with your doctor for rectal prolapse treatment.
How many types of Rectal Prolapse are there?
An individual may experience the following three types of rectal prolapse conditions:
- Internal Prolapse – In this condition, the rectum begins to drop, however, it is not yet dropping out of the anus.
- External Prolapse – The whole rectum drops of the anus.
- Mucosal Prolapse – A section of the rectal lining sneaks out of the anus.
How to identify the Rectal Prolapse Symptoms?
An individual may feel like sitting on a ball after bowel movements or you may feel like something is handing out of your anus, that could be a rectal prolapse.
You may experience rectal prolapse first time after passing the stools. In the first few intervals, you may feel the rectum has moved back to its place. As the days move on, you may experience something that has come out of the body, and something down there is not normal. In this condition, you might be able to push the rectum back in.
There are other rectal prolapse symptoms that include:
- Feeling of something handing out of the anus.
- Pain and bleeding from the rectum.
- Leaking of blood, stools, or mucus from your anus.
- A red mass is visible outside the anus.
Initially, rectal prolapse may appear like hemorrhoids handing out of the anus. However, these are two distinct medical conditions. Hemorrhoids are swollen blood veins in the lower part of the rectum that may trigger pain, bleeding, itching after bowel movements. Your PCP can help diagnose if you have hemorrhoids or rectal prolapse.
What are the Rectal Prolapse Causes?
There are various factors that can cause rectal prolapse, that include:
- Applying pressure or straining during bowel movements for a long time.
- Experiencing diarrhea or constipation problem for a long time.
- Old injury or surgery at hip areas or to the anal area.
- Weak muscles and ligaments in the rectal region due to old age.
- Neurological issues, like spinal cord transection or spinal cord ailment.
- Damage to nerves that have created an impact on muscles’ ability to loosen and tighten due to normal delivery complications, pregnancy, injury to the spine, or anal sphincter paralysis.
What are the Rectal Prolapse Risk Factors?
Women are more prone to rectal prolapse than men, particularly females over the age of 50 years. People who are old and have a history of prolonged constipation or issues with the pelvic area are at higher risk of developing rectal prolapse.
The following health conditions can also develop the risk of rectal prolapse:
- Pelvic floor or anus muscle weakness due to old age
- Congenital bowel disorders such as Intestinal neuronal dysplasia (IND) or Hirschsprung’s disease
- Family history of rectal prolapse
- Parasitic diseases such as schistosomiasis
- COPD – Chronic Obstructive Pulmonary Disorder
- Chronic constipation
- Benign prostatic hypertrophy
- Lower back injury or disc ailment
- Putting pressure during bowel movements
- Ligament injury or problem that connects the rectum to the intestinal wall
How to diagnose rectal prolapse?
Rectal prolapse diagnosis includes a rectal examination. Consult with your doctor to conduct for detailed examination of the rectum, which may include:
- Anal sphincter electromyography (EMG): This examination helps identify any nerve damage or anal muscle (sphincter) issue.
- Colonoscopy: It is used to examine any changes or deformities in the large intestines (colon) and the rectum by inserting a small camera fitted on a long tube at the rear end.
- Anal Ultrasound: The physician inserts a probe in the anus and rectum to examine the muscles and tissues.
- Proctography: It is an X-ray of the rectum and muscle of the pelvic floor.
- Pudendal nerve terminal motor latency test (PNTML): It is a standard proposal for the examination of fecal incontinence.
- MRI: It is used to examine all the organs in the pelvic region.
- Anorectal manometry: This examination is conducted to check the functionality and ability of the rectum and anal sphincter to pass the stools.
- Proctosigmoidoscopy: In this test, a long tube with a camera on the top is inserted at the rear-end to examine the intestines for any inflammation, tumor, or scarring.
How to treat rectal prolapse?
According to Dr. Valeria Simone MD, board-certified general surgeon at Southlake General Surgery, Texas, the most recommended procedure for Rectal prolapse treatment is surgery to place the rectum back in place. There are various methods in surgery that your PCP can suggest after the examination of your overall health, present condition, and age. There are two recommended methods of surgery, that include:
- Abdominal Surgery: In this surgical procedure, the surgeon makes one large incision or uses laparoscopic surgery that includes small incisions to insert the laparoscope along with a special surgical instrument and fix the problem.
- Perineal: It is also known as rectal repair. This procedure is recommended for individuals who are old or have other medical issues. This surgery may include the inner lining of the rectum or the part of the rectum stretching out of the anus.
Prevention of Rectal Prolapse
An individual needs to take precautions such as not to strain during bowel movements for rectal prolapse prevention. You can also try the following suggestion to reduce or prevent constipation that prompts straining during bowel movements:
- Take a fiber-rich diet that includes fresh fruits and vegetables.
- Drink plenty of water and fresh fruit juice.
- Daily workout and maintain a healthy weight.
- In case of constipation, speak to your doctor to suggest stool softeners.
- Avoid lifting heavy objects that put pressure on the bowel muscles.
What are the complications of rectal prolapse?
An individual may experience the following rectal prolapse complications if it is not treated:
- Unable to push the rectum inside by yourself
- Damage to rectum such as bleeding or ulceration
- Gangrene, or the strangulation of rectal tissues
- Strangulation, or obstruction of blood circulation in the rectum
Appointment
To know more about the Rectal Prolapse – causes, symptoms, diagnosis, treatment, and consultation. You can contact our healthcare expert today at +1 (817) 748-0200. You can also make an online appointment with us.