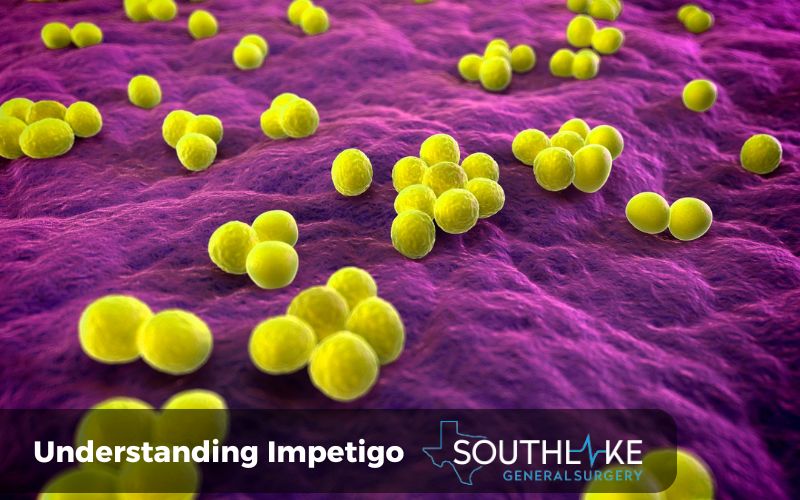
Impetigo infection is a common skin infection that primarily affects young children, although it can also occur in adults. It is caused by bacteria, most commonly Staphylococcus aureus (staph) and Streptococcus pyogenes (strep). Impetigo is extremely contagious and can be transmitted easily through direct skin-to-skin contact or by sharing personal items like towels or clothing.
The infection typically starts when the bacteria enter the skin through a cut, scratch, insect bite, or other skin condition. The bacteria then multiply and cause inflammation and infection in the top layers of the skin, resulting in the characteristic sores and blisters associated with impetigo.
Impetigo can present in different forms, including non-bullous impetigo, bullous impetigo, and ecthyma. Non-bullous impetigo is the most common type and is characterized by itchy sores that quickly burst, leaving behind a honey-colored crust. Bullous impetigo involves larger, fluid-filled blisters that eventually break open and form crusts. Ecthyma is a more severe form of impetigo that can cause painful blisters and open sores that may lead to scarring.
Prompt treatment is essential to prevent the spread of impetigo and to alleviate symptoms. Antibiotics, both topical and oral, are commonly prescribed to help clear the infection. In addition to treatment, practicing good hygiene and taking preventive measures can help reduce the risk of impetigo.
Key Highlights
- Impetigo is a prevalent bacterial skin infection that primarily impacts young children.
- The infection is caused by bacteria like Staphylococcus aureus (staph) and Streptococcus genus (strep).
- Impetigo causes sores and blisters on the skin, which can be itchy and painful.
- Treatment for impetigo includes antibiotics, both topical and oral, to help clear the infection.
- Prevention techniques for impetigo include practicing good hygiene, avoiding skin contact, and maintaining clean environments.
- Complications of untreated impetigo can include the spread of infection to other parts of the body and long-term health implications.
Understanding Impetigo
Impetigo is a bacterial skin infection that primarily affects young children, although adults can also be affected. There are two primary forms of impetigo: non-bullous impetigo and bullous impetigo. The bacteria
Staphylococcus aureus is what causes non-bullous impetigo, which is the most prevalent type. It typically starts with the development of itchy sores that quickly burst and form a honey-colored crust.
Bullous impetigo, on the other hand, is less common and is characterized by larger fluid-filled blisters. Both types of impetigo can be treated with antibiotics.
Defining Impetigo in Clinical Terms
Impetigo is a bacterial skin infection that affects the outer layers of the skin, known as the epidermis. The bacteria Staphylococcus aureus and Streptococcus pyogenes are responsible for it.
Bullous impetigo is a specific type of impetigo characterized by the formation of large, fluid-filled blisters on the skin. These blisters are caused by the release of toxins from the bacteria.
Non-bullous impetigo, on the other hand, is the more common type and is characterized by the formation of itchy sores that quickly burst and form a honey-colored crust.
Both types of impetigo can be contagious and are typically treated with antibiotics to clear the infection.
The Epidemiology of Impetigo
Impetigo is a common skin infection, especially among young children. It is estimated that impetigo accounts for about 10% of skin conditions in children. This infection is more prevalent in warm months when children spend more time outdoors and have increased exposure to bacteria.
Impetigo is very contagious and can be easily transmitted through direct skin contact or by sharing personal items like towels or clothing. Close contact with an infected individual, such as living in the same household or attending daycare, increases the risk of contracting impetigo.
Additionally, certain factors, such as having cuts, insect bites, or other skin conditions, can also increase the risk of impetigo.
Identifying Impetigo Symptoms
Impetigo is characterized by the presence of sores and blisters on the skin. The main symptoms of impetigo include:
- Itchy sores that may be red or pink in color
- Blisters that can burst and form a yellowish crust
- Crusty or oozing sores
- Redness and inflammation around the affected areas
- Swollen lymph nodes near the sores
These symptoms usually develop within a few days of the bacteria infecting the skin. Impetigo can occur on any part of the body but is mostly found around the mouth and nose.
Early Signs and Progression
The early signs of impetigo typically involve the development of redness and inflammation on the skin. This is followed by the formation of blisters, which can be filled with fluid or pus. These blisters may burst and form a crust or scab.
If left untreated, impetigo can progress and lead to the spread of infection to other areas of the body. It is important to seek prompt treatment to prevent the infection from worsening and to alleviate symptoms. Intervening early can prevent complications and speed up the recovery process.
Visual Guide to Impetigo Lesions
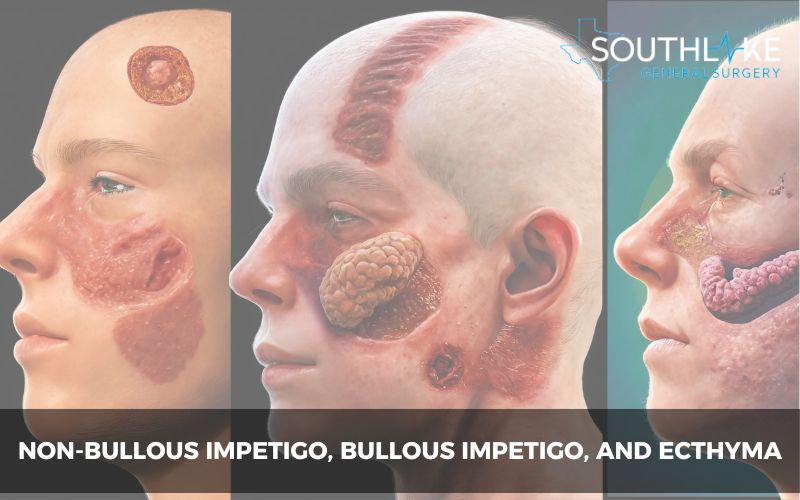
Impetigo lesions can vary in appearance depending on the stage of infection and the type of impetigo. Here is a visual guide to help you recognize impetigo sores:
- Non-bullous impetigo: The initial stage is characterized by the development of small blisters or sores that quickly burst and form a crust. The affected areas may be red or pink in color and can be itchy. Crusty yellow or golden scabs may form as the skin heals, and they eventually fade without leaving scars.
- Bullous impetigo: The lesions in bullous impetigo are larger and filled with fluid. They may appear clear or translucent and do not show redness or inflammation around the surrounding skin. As the blisters break open, crusty sores form, and the skin heals without scarring.
- Ecthyma: This severe form of impetigo involves painful blisters that can turn into ulcers. The affected areas may have thick crusts and redness near the surrounding skin. Scarring may occur as the infection goes deeper into the skin.
Causes and Risk Factors

Impetigo is caused by bacteria, specifically Staphylococcus aureus and Streptococcus pyogenes. These bacteria can enter the skin through cuts, scratches, insect bites, or other skin conditions.
Impetigo is highly contagious and can spread through direct skin-to-skin contact or by sharing personal items such as towels or clothing.
Certain risk factors can increase the likelihood of developing impetigo, including close contact with infected individuals, compromised immune system, and underlying skin conditions. It is important to take preventive measures to reduce the risk of impetigo.
Bacterial Culprits Behind Impetigo
Impetigo is primarily caused by two types of bacteria: Staphylococcus aureus (staph) and Streptococcus pyogenes (strep). These bacteria are commonly found on the skin and can enter the body through cuts, scratches, insect bites, or other skin conditions.
Staphylococcus aureus is responsible for about 80% of non-bullous impetigo cases, while Streptococcus pyogenes accounts for about 10%.
Both types of bacteria can multiply and cause inflammation and infection in the top layers of the skin, resulting in impetigo. Prompt treatment with antibiotics is essential to clear the infection and prevent complications.
Who is Most at Risk?
Certain individuals may be more susceptible to impetigo due to various risk factors. The table below outlines the groups of people who are most at risk:
Risk Factors with Examples:
- Young Children – Preschoolers and toddlers
- Close contact with infected person – Siblings, classmates, daycare contacts
- Weakened immune system – Individuals with HIV/AIDS, diabetes, or cancer
- Skin conditions or infections – Eczema, dermatitis, insect bites
- Living in crowded or close quarters – Dormitories, military barracks, sports teams
Young children, especially those in daycare or school settings, are at a higher risk of impetigo due to close contact with other children and the prevalence of the bacteria in these environments.
Individuals with weakened immune systems, such as those with HIV/AIDS or certain medical conditions, may also be more susceptible to impetigo. Additionally, skin conditions or infections can increase the risk of impetigo.
Diagnosis of Impetigo Infection
To diagnose impetigo infection, a healthcare professional, will examine the affected areas of the skin. They will look for characteristic signs such as sores, blisters, and crusts.
In some cases, they may also take a sample of the fluid from one of the sores to send to a laboratory for testing. This can help determine the specific bacteria causing the infection and guide the choice of appropriate antibiotics.
A professional diagnosis is important to ensure accurate identification and appropriate treatment of impetigo.
Professional Diagnosis Procedures
A healthcare professional can diagnose impetigo through a visual examination of the skin. They will look for characteristic signs such as the presence of sores, blisters, and crusts.
In some cases, they may take a bacterial culture by collecting a sample of the fluid or crusted material from the affected area. This culture can help identify the specific bacteria causing the infection and determine the most effective antibiotics for treatment.
Additionally, the healthcare professional may inquire about any recent cuts, insect bites, or skin conditions that may have contributed to the development of impetigo. A professional diagnosis is essential to ensure accurate identification and appropriate treatment of impetigo.
Understanding Your Diagnosis
If you are diagnosed with impetigo, your healthcare provider will discuss the recommended treatment options with you. The primary treatment for impetigo is antibiotics, either topical or oral, depending on the severity of the infection.
Topical antibiotics, such as mupirocin ointment, are applied directly to the affected area, while oral antibiotics, such as amoxicillin, may be prescribed for more widespread or severe cases.
It is important to follow your healthcare provider’s instructions and complete the full course of antibiotics to ensure effective treatment.
In some cases, individuals with underlying health conditions or compromised immune systems may require additional medical management to prevent complications. Your healthcare provider will provide guidance on managing your impetigo and any associated health conditions.
Comprehensive Treatment Strategies

The comprehensive treatment of impetigo typically involves a combination of topical and oral antibiotics, along with home care measures. The treatment strategies may include:
- Topical antibiotic cream or ointment: These are applied directly to the affected areas to kill the bacteria and promote healing. Examples include mupirocin ointment.
- Oral antibiotics: For more severe cases or widespread infections, oral antibiotics may be prescribed to help clear the infection from within the body. Commonly prescribed oral antibiotics include amoxicillin and cephalosporins.
- Home remedies and care: Good hygiene practices, such as cleansing the affected areas with gentle soap and warm water, can help prevent the spread of infection. Applying warm compresses to the sores can provide relief and promote healing.
It is important to follow the prescribed treatment plan and complete the full course of antibiotics to ensure effective treatment and prevent the recurrence of impetigo.
Medications and Topical Treatments
Medication options for impetigo include both topical treatments and oral antibiotics. Topical treatments are usually the first line of defense for mild cases of impetigo. They include:
- Antibiotic ointment: Mupirocin ointment is commonly prescribed and applied directly to the affected areas of the skin. It helps to kill the bacteria causing the infection and promote healing.
- Topical antibiotics: In some cases, a healthcare professional may prescribe topical antibiotics, such as fusidic acid or retapamulin. These medications are applied directly to the skin and help to eliminate the bacteria causing the impetigo infection.
If the impetigo infection is more severe or widespread, oral antibiotics may be necessary. These medications are taken by mouth and help to eliminate bacteria from within the body.
Examples of oral antibiotics commonly used to treat impetigo include amoxicillin, cephalexin, and clindamycin. In cases where methicillin-resistant Staphylococcus aureus (MRSA) is suspected, alternative antibiotics such as trimethoprim-sulfamethoxazole or clindamycin may be prescribed.
Home Remedies and Care
In addition to prescribed medications, there are several home remedies and care measures that can help alleviate symptoms and promote healing in cases of impetigo. These include:
- Good hygiene practices: Regularly washing the affected areas with gentle soap and warm water can help remove crusts and prevent the spread of infection.
- Hot water compresses: Applying warm compresses to the sores can help soothe discomfort and promote healing.
- Natural remedies: Some natural remedies, such as tea tree oil or diluted apple cider vinegar, may have antibacterial properties and can be applied topically to the affected areas. Before using any natural remedies, it is crucial to consult with a healthcare professional to verify their safety and effectiveness.
It is important to note that while home remedies and care measures can provide relief, they should not replace prescribed medications or medical treatment for impetigo.
Prevention Is Better Than Cure
Preventing impetigo is essential to avoid the discomfort and inconvenience of the infection. Here are some effective prevention techniques:
- Practice good hygiene: Regularly washing your hands with soap and water, especially after touching potentially contaminated surfaces, can help prevent the spread of bacteria.
- Avoid skin contact: Minimize close contact with individuals who have impetigo or other contagious skin conditions.
- Maintain clean environments: Keep your living spaces clean and ensure that personal items such as towels, clothing, and bedding are washed regularly.
- Lifestyle adjustments for risk reduction: Strengthening your immune system through a healthy diet, regular exercise, and adequate sleep can help reduce the risk of impetigo.
By adopting these prevention techniques, you can minimize the risk of impetigo and promote overall skin health.
Effective Prevention Techniques

Preventing impetigo involves practicing good hygiene and taking precautions to avoid skin contact with infected individuals or contaminated surfaces. Here are some effective prevention techniques:
- Hand washing: Regularly wash your hands with soap and water, especially after touching potentially contaminated surfaces or coming into contact with individuals who have impetigo.
- Avoiding skin contact: Minimize close contact with individuals who have impetigo or other contagious skin conditions. This includes avoiding sharing personal items such as towels, clothing, or bedding.
- Clean environments: Ensure that your living spaces are clean and hygienic. Regularly wash towels, clothing, and bedding in hot water to kill any bacteria that may be present.
By following these prevention techniques, you can reduce the risk of impetigo and maintain good skin health.
Lifestyle Adjustments for Risk Reduction
Making lifestyle adjustments can help reduce the risk of impetigo and promote overall skin health. Here are some lifestyle changes that can contribute to risk reduction:
- Strengthening the immune system: A strong immune system can help protect against bacterial infections. To uphold a healthy lifestyle, consume a well-rounded diet, engage in consistent physical activity, and prioritize sufficient sleep.
- Diet: Consume a diet rich in fruits, vegetables, whole grains, and lean proteins to support immune function and overall health.
- Exercise: Regular physical activity can boost the immune system and promote good overall health.
By incorporating these lifestyle adjustments into your routine, you can help reduce the risk of impetigo and maintain optimal skin health.
Living and Managing with Impetigo
Living with impetigo may require some adjustments to daily life to manage the infection effectively. Here are some tips for living and managing with impetigo:
- Personal care: Practice good hygiene, such as regularly washing your hands, cleaning the affected areas, and avoiding scratching the sores.
- Activity modifications: Depending on the severity and location of the impetigo, you may need to modify certain activities to prevent the spread of infection or to avoid discomfort.
- Impetigo management: Follow the prescribed treatment plan, including taking antibiotics as directed and keeping the affected areas clean and protected.
With proper management and adherence to treatment, impetigo can be effectively controlled and eventually cleared.
Daily Life and Activity Modifications
Living with impetigo may require making certain adjustments to daily life and activities. Here are some considerations:
- School and work: It is important to inform school or work authorities about the impetigo infection to prevent the spread of the bacteria. Depending on the severity and location of the infection, you may need to stay home until the sores have healed or until you are no longer contagious.
- Personal care: Avoid sharing personal items such as towels, clothing, or bedding to prevent the spread of infection. Practice good hygiene by regularly washing your hands and keeping the affected areas clean.
- Activity modifications: Depending on the location of the impetigo sores, you may need to avoid activities that could irritate or worsen the infection, such as swimming or contact sports.
By following these guidelines and making necessary modifications, you can effectively manage impetigo and minimize its impact on daily life.
When to Seek Further Medical Care
While impetigo is generally a mild and self-limiting infection, there are certain situations where further medical care may be necessary. Seek medical attention if:
- The infection worsens or spreads, despite following the prescribed treatment.
- You experience complications, such as cellulitis (infection of deeper skin layers), or signs of systemic infection.
- You develop symptoms of complications, such as rheumatic fever or glomerulonephritis.
- The infection does not improve within a week of starting treatment.
It is important to promptly address any concerns or complications related to impetigo to ensure appropriate management and prevent further complications.
Potential Complications and Risks
Although impetigo is generally a mild infection, untreated impetigo can lead to potential complications and long-term health implications. Some of the possible complications include:
- Spread of infection: Untreated impetigo can lead to the spread of infection to other areas of the body or to other individuals through direct contact.
- Skin damage and scarring: Without proper treatment, impetigo can cause skin damage and scarring, especially in severe or deep cases.
- Long-term health implications: In rare cases, untreated impetigo can lead to complications such as glomerulonephritis (kidney inflammation) or rheumatic fever.
Prompt treatment and proper management of impetigo can help prevent these complications and minimize any long-term health implications.
Recognizing Severe Cases
While impetigo is generally a mild infection, in some cases, it can become more severe. Ecthyma is a severe form of impetigo that penetrates deeper layers of the skin. It is characterized by the formation of painful blisters that can turn into ulcers.
Other signs of severe impetigo can include redness and inflammation around the affected areas and the presence of systemic symptoms such as fever or malaise.
It is crucial to promptly seek medical attention if you observe any of these signs or symptoms. Severe cases of impetigo may require more intensive treatment and management to prevent complications and promote healing.
Long-Term Health Implications
While impetigo is typically a self-limiting infection, there can be potential long-term health implications if it is not treated properly. Some of these long-term implications may include:
- Kidney problems: In rare cases, untreated impetigo can lead to kidney problems, such as glomerulonephritis. This is a condition where the kidneys become inflamed and can result in complications such as high blood pressure and blood in the urine.
- Scar tissue: If impetigo sores are not properly cared for or if there are complications, they can lead to the formation of scar tissue.
- Reinfection: Without proper treatment, impetigo can persist or recur, leading to a higher risk of reinfection.
It is important to seek medical attention and follow the prescribed treatment to prevent the long-term health implications associated with impetigo.
Outlook
The outlook for impetigo is generally good with prompt treatment and proper management. Most cases of impetigo resolve within 7–10 days with antibiotics and appropriate care. Completing the entire course of antibiotics is crucial to ensuring the complete clearance of the infection.
By practicing good hygiene, maintaining a healthy lifestyle, and taking preventive measures, the risk of impetigo can be minimized. Regular follow-up with a healthcare professional can help monitor the condition and address any concerns or complications that may arise.
Make an Appointment
If you suspect that you or your child has impetigo, it is important to make an appointment with our healthcare professional at +1 (817) 748-0200. They have the ability to offer a precise diagnosis and suggest the correct treatment plan. Prompt treatment can help alleviate symptoms, prevent the spread of infection, and minimize the risk of complications.
Additionally, a healthcare professional can provide guidance on preventive measures to reduce the risk of impetigo. Don’t hesitate to reach out to a healthcare professional for any concerns or questions regarding impetigo.
Frequently Asked Questions
Can Impetigo return after treatment?
Yes, impetigo can recur even after receiving antibiotic treatment. To prevent recurrence, it is important to follow good hygiene practices, such as regularly washing your hands and keeping the affected areas clean. Maintaining good overall hygiene and avoiding close contact with infected individuals can also help reduce the risk of recurrent impetigo.
How Do You Differentiate Between Impetigo and Other Skin Conditions?
Differentiating between impetigo and other skin conditions can be challenging. However, impetigo is characterized by the presence of sores, blisters, or crusts on the skin. A healthcare professional can provide a clinical diagnosis based on the visual symptoms and other diagnostic tests, if necessary.
Are there any new advances in impetigo treatment?
Research is ongoing to explore new treatments for impetigo. However, the current primary treatment remains antibiotics. It is important to use antibiotics appropriately and as prescribed to prevent antibiotic resistance. Talk to your healthcare professional for the latest information on impetigo treatment options.
Medically Reviewed By: Dr. Valeria Simone MD
Board-certified General Surgeon at Southlake General Surgery, Texas, USA.
Follow us on Facebook and YouTube.
References:
- Taylor, Tracey A., and Chandrashekhar G. Unakal. “Staphylococcus Aureus Infection.” StatPearls – NCBI Bookshelf, 17 July 2023, www.ncbi.nlm.nih.gov/books/NBK441868.
- Wallace, Heather A., and Thomas B. Perera. “Necrotizing Fasciitis.” StatPearls – NCBI Bookshelf, 21 Feb. 2023, www.ncbi.nlm.nih.gov/books/NBK430756.
- Orchard A, van Vuuren S. Commercial Essential Oils as Potential Antimicrobials to Treat Skin Diseases. Evid Based Complement Alternat Med. 2017;2017:4517971. https://doi:10.1155/2017/4517971
- Ross, Adam, and Hugh W. Shoff. “Staphylococcal Scalded Skin Syndrome.” StatPearls – NCBI Bookshelf, 25 July 2023, www.ncbi.nlm.nih.gov/books/NBK448135.
- Nardi, Naomi M., and Timothy J. Schaefer. “Impetigo.” StatPearls – NCBI Bookshelf, 31 July 2023, www.ncbi.nlm.nih.gov/books/NBK430974.
- Ross, Adam, and Hugh W. Shoff. “Toxic Shock Syndrome.” StatPearls – NCBI Bookshelf, 7 Aug. 2023, www.ncbi.nlm.nih.gov/books/NBK459345.
- Brazel, Morgan, et al. “Staphylococcal Scalded Skin Syndrome and Bullous Impetigo.” Medicina, vol. 1157, no. 11, 24 Oct. 2021, https://doi.org/10.3390/medicina57111157.
- Hartman-Adams, Holly, et al. “Impetigo: Diagnosis and Treatment.” AAFP, 15 Aug. 2014, www.aafp.org/pubs/afp/issues/2014/0815/p229.html.
- Ayi, Bertha. “Streptococcal Infections (Groups a and B).” Elsevier eBooks, vol. 1–10, 1 Jan. 2007, https://doi.org/10.1016/b978-008055232-3.60852-9.

