Crohn’s disease and hemorrhoids are two separate conditions that can affect the gastrointestinal tract. While they are distinct conditions, they are linked, especially for patients with Crohn’s disease. Understanding these conditions and their impact on the digestive system is crucial for managing and treating them effectively.
Any area of the gastrointestinal system, from the mouth to the anus, can be impacted by Crohn’s disease, a chronic inflammatory bowel disease (IBD). It is characterized by chronic inflammation and can lead to various symptoms, including abdominal pain, diarrhea, weight loss, and deep ulcers.
The exact cause of Crohn’s disease is unknown, but it is believed to involve a combination of genetic factors, an abnormal immune response, and environmental triggers.
Hemorrhoids, on the other hand, are swollen veins in the anal canal and rectum. They can be internal or external and are often caused by increased pressure in the anal area. Common symptoms of hemorrhoids include rectal bleeding, pain, itching, and discomfort.
While hemorrhoids can affect anyone, individuals with Crohn’s disease are at a higher risk of developing them due to the inflammation and increased pressure in the anal region.
In this blog, we will delve into the details of Crohn’s disease and hemorrhoids, including their causes, symptoms, diagnosis, treatment options, and management strategies. We will also explore the link between these two conditions and provide insights into how they can be effectively managed for improved quality of life.
Key Highlights
- Crohn’s disease and hemorrhoids are both conditions that affect the gastrointestinal tract.
- Crohn’s disease is a chronic inflammatory bowel disease that can affect part of the digestive system.
- Hemorrhoids, on the other hand, are swollen veins in the anal canal and rectum.
- There is a link between Crohn’s disease and hemorrhoids, as patients with Crohn’s disease have a higher risk of developing hemorrhoids.
- Diagnosis of Crohn’s disease and hemorrhoids involves various diagnostic tests, such as colonoscopy and physical examination.
- Treatment options for Crohn’s disease include medication management and surgical interventions, while managing hemorrhoids in Crohn’s patients involves conservative treatments and, in some cases, surgical options.
What is Crohn’s Disease?
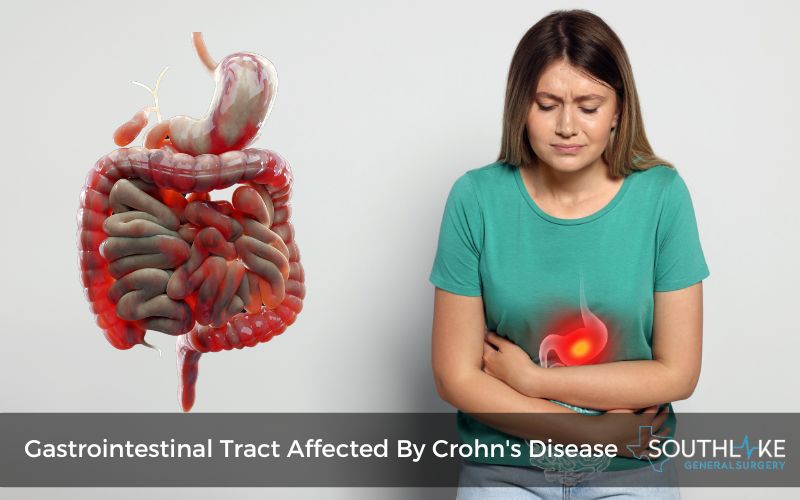
Inflammation of the digestive tract is the main symptom of Crohn’s disease, a chronic inflammatory disorder. It causes inflammation and damage to the gastrointestinal lining, leading to various symptoms like abdominal pain, diarrhea, fatigue, and weight loss. To effectively handle it, one must understand its nature.
Crohn’s disease is characterized by deep ulcers, which can result in complications like fistulas and abscesses. It differs from ulcerative colitis in that it can involve any part of the digestive system, not just the colon.
This disease typically manifests in episodes of flare-ups followed by periods of remission. It requires ongoing management and treatment to control symptoms and prevent complications.
Signs and Symptoms of Crohn’s Disease

Crohn’s disease manifests through a variety of signs and symptoms that can vary in severity and location along the digestive tract.
Common indications include:
- abdominal pain
- persistent diarrhea
- weight loss
- fatigue
Patients may also experience:
- rectal bleeding
- fever
- the formation of fistulas and abscesses
Notably, Crohn’s disease can lead to complications outside the gastrointestinal tract, such as inflammation in the joints, eyes, or skin. Monitoring these symptoms is crucial for timely intervention and management.
How Crohn’s Disease Affects the Digestive System
Crohn’s disease impacts the digestive system by causing inflammation along the gastrointestinal tract, particularly in the small intestine. This chronic condition leads to deep ulcers and can affect any part of the digestive tract, from the mouth to the anus.
In Crohn’s patients, the abnormal immune response results in complications such as diarrhea, abdominal pain, weight loss, and malnutrition.
Recent studies suggest a higher risk of developing complications like abscesses and fistulas. Understanding how Crohn’s disease affects the digestive system is crucial for effective management and treatment options.
Understanding Hemorrhoids
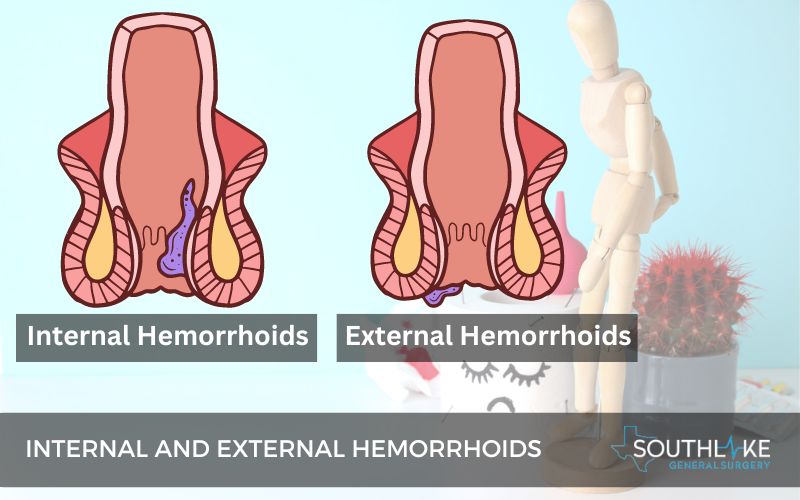
Hemorrhoids, or piles, refer to the enlargement of veins in the lower rectum and anus. They may be located inside the rectum or outside, beneath the skin surrounding the anus.
Hemorrhoids are common in the general population but can be more prevalent in individuals with Crohn’s disease and other inflammatory bowel diseases. Symptoms may include:
- pain
- itching
- bleeding
Understanding the link between Crohn’s disease and hemorrhoids is essential for effective management, as both conditions can impact the gastrointestinal tract and require tailored treatment approaches.
The Basics of Hemorrhoids
Hemorrhoids, or piles, are engorged blood vessels located in the rectum and anus that can result in pain and bleeding. They are a common condition among adults, especially in those who strain during bowel movements or are pregnant.
The two main types of Hemorrhoids are:
- internal hemorrhoids, which form inside the rectum where there are few pain-sensing nerves.
- external hemorrhoids, which form under the skin around the anus and can be more painful.
Hemorrhoids can be managed with lifestyle changes, over-the-counter treatments, and, in some cases, medical procedures.
Link Between Crohn’s Disease and Hemorrhoids
Crohn’s disease and hemorrhoids share common ground through inflammatory processes that affect the gastrointestinal tract. Patients with Crohn’s disease are at a higher risk of developing symptomatic hemorrhoids due to chronic inflammation in the region.
Recent studies have highlighted this relationship, underscoring the complexities of managing perianal disease in conjunction with Crohn’s.
Complications such as anal fissures and fistulas can further exacerbate the connection between the two conditions, necessitating a multidisciplinary approach to comprehensive care.
Causes and Risk Factors
Crohn’s disease and hemorrhoids have distinct causes and risk factors. Crohn’s disease results from an abnormal immune response, causing inflammation in the gastrointestinal tract, particularly the small intestine. Genetic predisposition and environmental factors play significant roles in triggering Crohn’s disease.
On the other hand, hemorrhoids are often linked to increased pressure on rectal veins from straining during bowel movements, obesity, or pregnancy. Individuals with Crohn’s disease are at a higher risk of developing symptomatic hemorrhoids due to chronic inflammation in the anal canal.
Genetic and Environmental Triggers for Crohn’s Disease
Crohn’s disease is influenced by genetic and environmental factors. Genetic predisposition plays a significant role in the development of this inflammatory bowel disease.
Recent studies have highlighted specific gene mutations associated with Crohn’s disease, contributing to abnormal immune responses within the gastrointestinal tract.
Environmental triggers such as diet, stress, and smoking also play a crucial role in triggering and exacerbating Crohn’s symptoms.
Early identification of these triggers can aid in personalized treatment plans for individuals with Crohn’s disease.
Risk Factors for Developing Hemorrhoids
Hemorrhoids affect many individuals, with specific risk factors contributing to their development. Factors such as chronic constipation or straining during bowel movements increase the likelihood of hemorrhoids.
Obesity and a sedentary lifestyle can also play a role in their occurrence. Pregnant women are at higher risk due to increased pressure on the abdomen.
Additionally, aging can weaken the tissues supporting the veins in the rectum and anus, making older adults more susceptible to hemorrhoids.
Diagnosing Crohn’s Disease and Hemorrhoids
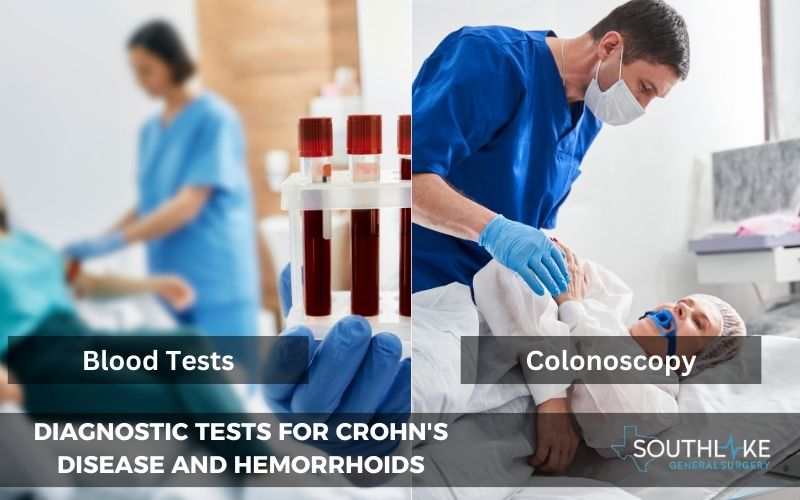
Diagnostic procedures play a pivotal role in identifying Crohn’s disease and hemorrhoids. For Crohn’s disease, healthcare providers commonly employ colonoscopy, blood tests, and imaging studies to confirm the diagnosis. These assessments help detect the characteristics of deep ulcers and inflammation in the gastrointestinal tract that are indicative of the condition.
On the other hand, diagnosing hemorrhoids often involves a visual examination of the rectal area, with additional tests like anoscopy or sigmoidoscopy if needed for conclusive evidence. The accuracy of these diagnostic methods ensures appropriate and timely management strategies for both conditions.
Diagnostic Tests for Crohn’s Disease
Diagnostic tests for Crohn’s disease play a pivotal role in accurate diagnosis. Various tests are employed to confirm the presence of the condition and assess its severity. Common diagnostics include:
- colonoscopy
- imaging tests like MRI/CT scans
- blood tests measuring inflammation markers
- stool tests to detect any abnormalities indicative of Crohn’s disease
Symptoms like inflammation or deep ulcers can be better identified with the use of endoscopic techniques that provide a clear view of the intestines.
Combining these tests enables healthcare providers to formulate an appropriate treatment plan for patients with Crohn’s disease.
Identifying Hemorrhoids: Methods and Criteria
Various methods are employed to identify hemorrhoids. Visual inspection of the anus and surrounding area is a common approach. Proctoscopy allows for a closer examination, while anoscopy provides a detailed view of the anal canal.
Criteria for diagnosing hemorrhoids include the presence of skin tags, visible swellings, and rectal veins. Symptoms such as anal pain, itching, and bleeding are considered indicative.
Healthcare providers also consider the medical history and the patient’s description of symptoms. These criteria help in accurately identifying hemorrhoids and initiating appropriate treatment.
Treatment Options for Crohn’s Disease
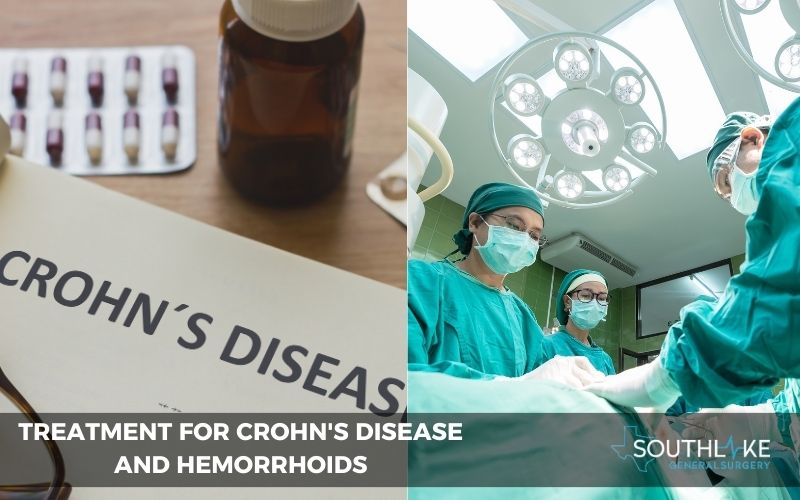
Crohn’s Disease treatment options vary depending on disease severity and individual response. Medications like anti-inflammatory drugs, immunosuppressants, and biologics are commonly prescribed to manage inflammation.
In cases of severe complications or resistance to medication, surgical intervention may be necessary. Surgical procedures can include removing damaged portions of the digestive tract or addressing complications such as fistulas or abscesses.
Patients need to work closely with healthcare providers to find the most effective treatment plan tailored to their specific conditions and symptoms.
Medication Management
Crohn’s disease treatment often involves medication management. Various drugs aim to reduce inflammation in the gastrointestinal tract, inducing and maintaining remission.
Medications such as aminosalicylates, corticosteroids, immunomodulators, and biologics are commonly prescribed to alleviate symptoms. Each type targets different aspects of the abnormal immune response that characterizes Crohn’s disease.
Medication choices depend on the severity of the condition, the patient’s response, and the presence of complications. Regular monitoring and adjustments by healthcare providers are crucial to ensure the most effective treatment for CD patients.
Surgical Interventions and Their Impact
Surgical interventions play a crucial role in managing Crohn’s disease and associated hemorrhoids. For Crohn’s disease patients, surgery becomes necessary in cases of complications like strictures or fistulas.
Surgical procedures aim to alleviate symptoms and improve the quality of life for individuals with severe conditions. Hemorrhoidectomy, a common procedure for symptomatic hemorrhoids, provides relief from pain and discomfort.
However, like any surgical intervention, there are potential risks and side effects to consider. Patients need to discuss the benefits and risks thoroughly with their healthcare provider before opting for surgical treatment.
Managing Hemorrhoids in Crohn’s Patients
For Crohn’s patients, managing hemorrhoids presents unique challenges due to the underlying inflammatory bowel disease. Conservative treatments, such as dietary modifications and fiber supplements, can help alleviate symptoms.
However, in cases where these methods are insufficient, surgical interventions may be necessary. It’s crucial to address hemorrhoids promptly in Crohn’s patients to prevent complications and improve overall quality of life.
By closely monitoring and managing hemorrhoidal symptoms in conjunction with Crohn’s disease, healthcare providers can tailor treatment plans to meet the individual needs of each patient.
Conservative Treatments and Lifestyle Changes
When managing Crohn’s disease and hemorrhoids, conservative treatments and lifestyle changes play a crucial role.
For Crohn’s disease, focusing on a healthy diet, stress management, and regular exercise can help reduce symptoms.
Incorporating high-fiber foods and staying hydrated is beneficial for managing hemorrhoids. Avoiding straining during bowel movements and maintaining good anal hygiene also aid in symptom relief.
Adhering to prescribed medications and following a tailored treatment plan is essential for optimal management of both conditions. Lifestyle modifications can greatly improve the quality of life for individuals dealing with Crohn’s disease and hemorrhoids.
When Surgery Becomes Necessary
In cases where conservative treatments fail to relieve severe hemorrhoids in Crohn’s patients, surgical intervention becomes a necessity.
Persistent symptoms such as anal fissures or skin tags that impact quality of life may require surgical procedures like hemorrhoidectomy or rubber band ligation.
For individuals with Crohn’s disease, especially those with severe complications or anal abscesses, surgery may be crucial to address the underlying issues and prevent further discomfort.
Surgical options are typically considered when all other methods have not provided adequate relief or when the patient’s health is at risk.
Living with Crohn’s Disease and Hemorrhoids
Living with Crohn’s disease and hemorrhoids can be challenging. Managing a chronic inflammatory bowel disease like Crohn’s requires careful attention to diet and nutrition to minimize flare-ups. Stress management plays a crucial role in maintaining overall well-being for individuals dealing with these conditions.
Additionally, seeking mental health support can help in coping with the emotional aspects of living with chronic illnesses. Understanding the symptoms and triggers specific to Crohn’s disease and hemorrhoids is vital for effective management and enhancing the quality of life for patients.
Diet and Nutrition Tips
To manage Crohn’s disease and hemorrhoids effectively, incorporating specific diet and nutrition tips is crucial. Consuming a well-balanced diet rich in fiber while avoiding trigger foods like spicy dishes can help alleviate symptoms associated with both conditions.
Opt for easily digestible foods and stay hydrated to support your digestive system. Including probiotics in your diet may also aid in maintaining gut health.
Additionally, vitamin- and mineral-rich foods can help prevent nutritional deficiencies common in individuals with inflammatory bowel diseases. Seeking professional guidance from a healthcare provider or a dietitian is advisable for a personalized dietary plan.
Stress Management and Mental Health Support
Stress management is crucial for individuals with Crohn’s Disease and hemorrhoids, given the impact of these conditions on mental health. The emotional toll of chronic illnesses can exacerbate symptoms and affect overall well-being.
Seeking mental health support through therapy or support groups can help manage stress levels. Techniques such as mindfulness, relaxation exercises, and maintaining a healthy lifestyle can also promote mental well-being.
It is essential to prioritize self-care and seek professional help when needed to navigate the challenges of living with these conditions.
The Role of Southlake General Surgery in Your Care
At Southlake General Surgery, we specialize in comprehensive care for patients with complex conditions like Crohn’s disease and hemorrhoids. Dr. Valeria Simone MD, leads our expert team, offering state-of-the-art surgical treatments tailored to individual needs.
Our focus on delivering personalized care ensures that patients receive the highest standard of treatment. From addressing anal fissures to managing symptomatic hemorrhoids in Crohn’s patients, our integrated approach aims to improve your quality of life.
Expert Care by Dr. Valeria Simone MD
Dr. Valeria Simone MD provides expert care for Crohn’s disease and hemorrhoids. As an experienced board-certified general surgeon, Dr. Simone offers comprehensive treatment options for patients with complex conditions. Her expertise in managing inflammatory bowel diseases, such as Crohn’s disease, ensures personalized care for everyone.
With a focus on surgical interventions and conservative treatments, Dr. Simone tailors her approach to meet the specific needs of CD patients. Trust in her experience to provide high-quality care and guidance throughout your treatment journey.
Why Choose Southlake General Surgery?
Choose Southlake General Surgery for expert care by Dr. Valeria Simone MD, providing advanced treatments with a focus on patient well-being. Benefit from personalized and comprehensive services for your Crohn’s Disease and Hemorrhoids management.
Conclusion
In conclusion, understanding Crohn’s Disease and Hemorrhoids is crucial for managing these conditions effectively. Recognizing the signs, symptoms, and treatment options can greatly impact your quality of life.
If you have concerns about Crohn’s Disease or Hemorrhoids, seeking professional medical guidance is essential. At Southlake General Surgery, under the expert care of Dr. Valeria Simone MD, you can receive personalized treatment and support tailored to your needs.
Make An Appointment
To schedule an appointment with Dr. Valeria Simone MD at Southlake General Surgery in Texas, USA, please contact our healthcare expert today at +1 (817) 748-0200. Dr. Simone specializes in surgical treatment for a range of conditions, including Crohn’s disease and hemorrhoids.
By contacting our clinic, you can access expert care tailored to your specific needs. Whether you require medical therapy, medication management, or surgical interventions for conditions related to the gastrointestinal tract, Dr. Simone and our team are here to provide comprehensive and compassionate care. Contact our healthcare expert today to book your appointment.
Frequently Asked Questions
What are the First Signs of Crohn’s Disease?
Early signs of Crohn’s disease include abdominal pain, diarrhea, fatigue, weight loss, and rectal bleeding. Recognizing these symptoms is crucial for timely diagnosis and management.
What is the best way to treat hemorrhoids in people with Crohn’s disease?
In Crohn’s patients, treating hemorrhoids involves managing both conditions simultaneously. Conservative measures like fiber-rich diet, sitz baths, and topical creams can help relieve hemorrhoidal symptoms. Surgery may be a possibility in more serious instances.
What Causes Crohn’s Disease Symptoms Like Anal Fissures and Hemorrhoids?
Crohn’s disease can lead to anal fissures and hemorrhoids due to inflammation in the digestive tract. The passing of hard stools, diarrhea, and the effects on blood vessels contribute to their development. Proper management of Crohn’s symptoms can help alleviate these issues.
Medically Reviewed By: Dr. Valeria Simone MD
Board-certified General Surgeon at Southlake General Surgery, Texas, USA.
Follow us on Facebook and YouTube.
References:
- “Hemorrhoids.” Piles | MedlinePlus, https://medlineplus.gov/hemorrhoids.html.
- McClane, Steven J., and John L. Rombeau. “Anorectal Crohn’s Disease.” the Surgical Clinics of North America/Surgical Clinics of North America, vol. 169–183, no. 1, 1 Feb. 2001, https://doi.org/10.1016/s0039-6109(05)70279-6.
- Lewis, Robert T., and David J. Maron. “Anorectal Crohn’s Disease.” the Surgical Clinics of North America/Surgical Clinics of North America, vol. 83–97, no. 1, 1 Feb. 2010, https://doi.org/10.1016/j.suc.2009.09.004.
- Cohen, Zane. “An Approach to Perirectal Disease in Inflammatory Bowel Disease.” Inflammatory Bowel Diseases, vol. 228–230, no. 3, 1 Aug. 1999, https://doi.org/10.1097/00054725-199908000-00011.
- McCloud, J.M., Jameson, J.S. and Scott, A.N.D. (2006), Life-threatening sepsis following treatment for hemorrhoids: a systematic review. Colorectal Disease, 8: 748-755. https://doi.org/10.1111/j.1463-1318.2006.01028.x
- Singh, B., et al. “Perianal Crohn’s Disease.” British Journal of Surgery, vol. 801–814, no. 7, 10 May 2004, https://doi.org/10.1002/bjs.4613.
- Gravié, Jean François, et al. “Stapled Hemorrhoidopexy Versus Milligan-Morgan Hemorrhoidectomy.” Annals of Surgery, vol. 29–35, no. 1, 1 July 2005, https://doi.org/10.1097/01.sla.0000169570.64579.31.
- Bandzar, Sean, et al. “Crohn’s Disease: A Review of Treatment Options and Current Research.” Cellular Immunology, vol. 45–52, no. 1–2, 1 Nov. 2013, https://doi.org/10.1016/j.cellimm.2013.11.003.
- Veauthier, Brian, and Jaime R. Hornecker. Crohn'S Disease: Diagnosis and Management. 1 Dec. 2018, www.aafp.org/pubs/afp/issues/2018/1201/p661.html.
- Lightner, Amy L., et al. “Excisional Hemorrhoidectomy: Safe in Patients With Crohn’s Disease?” Inflammatory Bowel Diseases, vol. 1390–1393, no. 9, 21 Oct. 2019, https://doi.org/10.1093/ibd/izz255.

